Neurological dysfunction following coronary artery bypass graft (CABG) surgery can manifest as stroke, encephalopathy including delirium and post-operative cognitive dysfunction. Stroke is one of the most devastating complications after CABG surgery, entailing permanent disability and a 3–6 fold increased risk of death with a case-fatality rate up to 20 %.1,2 It is also associated with incremental hospital resource consumption and a longer length of hospital stay. It has been estimated among a population of 114,233 Medicare beneficiaries that the occurrence of stroke entails an incremental cost of US$18,552 and an incremental length of hospital stay of seven days.3
The risk of stroke after CABG varies across studies ranging from 0.0 % to 5.2 %,4,5 depending on study design, patient risk profile, operative techniques and the length of study follow-up. Although advances in surgical, anaesthetic and medical management have occurred across the last 10 years, the risk of stroke after CABG has not significantly declined, likely because an older and sicker population is now deemed suitable to undergo CABG surgery.6
In addition, stroke represents a dismal point against CABG when deciding the optimal strategy of revascularisation between CABG and percutaneous coronary intervention (PCI) in patients with multivessel coronary artery disease. Specifically, in a recent meta-analysis including 19 randomised controlled trials with 10,944 patients, CABG was associated with significantly higher 30-day and one-year rates of stroke compared with PCI.7 Interestingly, the difference in the risk of stroke between the two strategies of revascularisation seemed more evident in patients with unprotected left main coronary artery disease or multivessel coronary artery disease than in patients with single vessel coronary artery disease.7 In addition, in a recently published meta-regression analysis including 20 randomised controlled trials comparing PCI versus CABG in patients with stable angina, a significant interaction between female gender and stroke risk reduction with PCI was apparent.8
Pathogenesis
The pathogenesis of stroke is multifactorial, but two variables are believed to play a major role – cerebral embolism and hypoperfusion during surgery. Some studies suggested that panvasacular inflammation may also play a role, especially in the setting of acute coronary syndromes.9 Cerebral embolism is by far the most common cause of peri-operative stroke accounting for 50–75 % of cases. Cerebral emboli arise from either the ascending aorta during surgical manipulation or from the heart due to atrial fibrillation.
The prevalence of atherosclerotic disease in the ascending aorta varies across studies, depending on the patient population, the criteria used to define the disease, and the diagnostic tool implemented to detect the disease, with case rates up to 38 % in some studies.10 This prevalence has significantly increased in recent years, likely due to better diagnostic methods and an increasing population of elderly. Peripheral vascular disease, age, hypertension and diabetes have been reported to be independent predictors of atherosclerotic disease of the ascending aorta.11
A high correlation between atherosclerosis of the ascending aorta and atheroembolism during CABG surgery has been established by several studies.5,12–14 In a prospective multicentre study including more than 2,000 patients, atherosclerosis of the ascending aorta was the strongest independent predictor of stroke associated with CABG.5 In the study by Bergman et al., extensive atherosclerotic disease of the ascending aorta was associated with a 31 % risk of post-operative stroke.12 The risk depends on the presence, location and extent of disease when the aorta is surgically manipulated.15
Embolisation of atheromatous debris from the aorta is likely to occur at the time of cannulation of the aorta for establishing cardiopulmonary bypass, when the aortic clamp is applied or released, or when proximal graft anastomoses are performed using side-biting clamp. Cerebral emboli often co-exist with intra-operative hypoperfusion, which impairs the clearance of microemboli16 and may be responsible of bilateral watershed infarcts after CABG.17 Cerebral hypoperfusion may be exacerbated by the co-existence of carotid artery stenosis, which is another important risk factor for intra-operative stroke.18
Chronic atrial fibrillation is a risk factor for cerebral embolism, and in patients undergoing CABG the peri-operative period may be at increased risk of stroke due to the necessity to modulate anticoagulant therapy. In addition, recent studies have suggested that new onset atrial fibrillation in the peri-operative period is also a risk factor for post-CABG stroke.19 Atrial fibrillation develops in 15–30 % of patients undergoing CABG,20,21 and although initial reports suggested that it was a self-limited phenomenon with no relevant clinical sequelae, a recent study including 8,058 patients undergoing CABG, suggested that new onset atrial fibrillation was associated with significantly higher rates of stroke and long-term mortality.19
Risk Stratification
Identification of vulnerable patients at increased risk of stroke before CABG is of paramount importance for the surgical decision-making approach and informed consent. The risk of stroke before CABG has been extensively scrutinised leading to the identification of several risk factors. Age, diabetes, hypertension, peripheral vascular disease, renal failure, left ventricular dysfunction and non-elective surgery have consistently been reported as risk factors of peri-operative stroke in patients undergoing CABG surgery.22,23 All these risk factors can be assessed before surgery, so the information can assist informed decision-making by patients, their family and their physicians. The combination of these variables has generated several risk stratification tools that can be implemented before surgery, to determine the individual probability of stroke in patients undergoing CABG.
In the Charlesworth score, generated from 33,000 consecutive patients undergoing isolated CABG, seven variables are integrated, including age, diabetes, left ventricular ejection fraction <40 %, female gender, priority of surgery, renal dysfunction and peripheral vascular disease.22 In the simpler model generated by McKhann et al. only three variables are considered: age, hypertension and history of stroke.6 More recently, Hornero et al. generated and validated a new risk model (Pack2 score), including priority of surgery, peripheral vascular disease, preoperative cardiac failure/left ventricular ejection fraction <40 % and chronic kidney failure.23 Interestingly, in patients with Pack2 score ≥2, off-pump CABG significantly reduced the risk of stroke compared with on-pump CABG, whereas no difference was apparent between the two strategies of revascularisation in patients with Pack2 score <2. Further studies should externally validate this score and assess whether it is useful in clinical practice to select the optimal strategy of revascularisation between on-pump and off-pump CABG in high-risk patients.
However, while these risk stratification tools are important because they factor the additive effect of several variables, they also share a major limitation in disregarding two important risk factors – atherosclerotic disease of the ascending aorta12 and pre-existing cerebrovascular disease.6 As the impact of these two factors on the risk of post-operative stroke is substantial, they should always be scrutinised before deciding the optimal strategy of coronary revascularisation.
Severe atherosclerosis of the ascending aorta is often an unexpected intra-operative finding during CABG, when preoperative risk stratification has not been accurate. It represents a challenge for the surgeon, who may need to change the operative strategy. A variety of methods can be used before surgery to diagnose severe atherosclerosis in the ascending aorta, including computed tomography scanning, transoesophageal echocardiography or magnetic resonance imaging. Intra-operative ultrasonographic scanning of the aorta can also be used to detect atherosclerotic changes in the entire ascending aorta. It is a rapid, safe and sensitive method, and some studies have reported that it is more accurate than both transoesophageal echocardiography14 and computed tomography in detecting atheromatous debris in the ascending aorta.24
Assessment of the neurological risk profile of patients before CABG is another essential step to make accurate risk stratification. The neurological profile of the patient should be carefully characterised, seeking for a history of stroke, the presence of initial neurocognitive disorders, or the presence of pre-existing cerebrovascular disease.6 Recent studies have also suggested that detection of cerebral ischaemia by magnetic resonance imaging before CABG is strongly associated with the risk of post-operative stroke.25,26 Screening of carotid artery disease with echo Doppler before CABG should also be performed, especially in high-risk patients.
The Value of Off-pump Coronary Artery Bypass Graft in Reducing the Risk of Stroke
The observation that atherosclerosis of the ascending aorta is a major determinant of stroke after CABG has led some investigators to advocate the use of off-pump CABG to reduce surgical manipulation of the aorta. Several studies have compared clinical outcomes of patients treated with on-pump versus off-pump CABG, and results have been controversial. In general, observational studies have consistently suggested an association between off-pump CABG and stroke reduction, but this association has not been confirmed in several randomised controlled trials (RCTs).
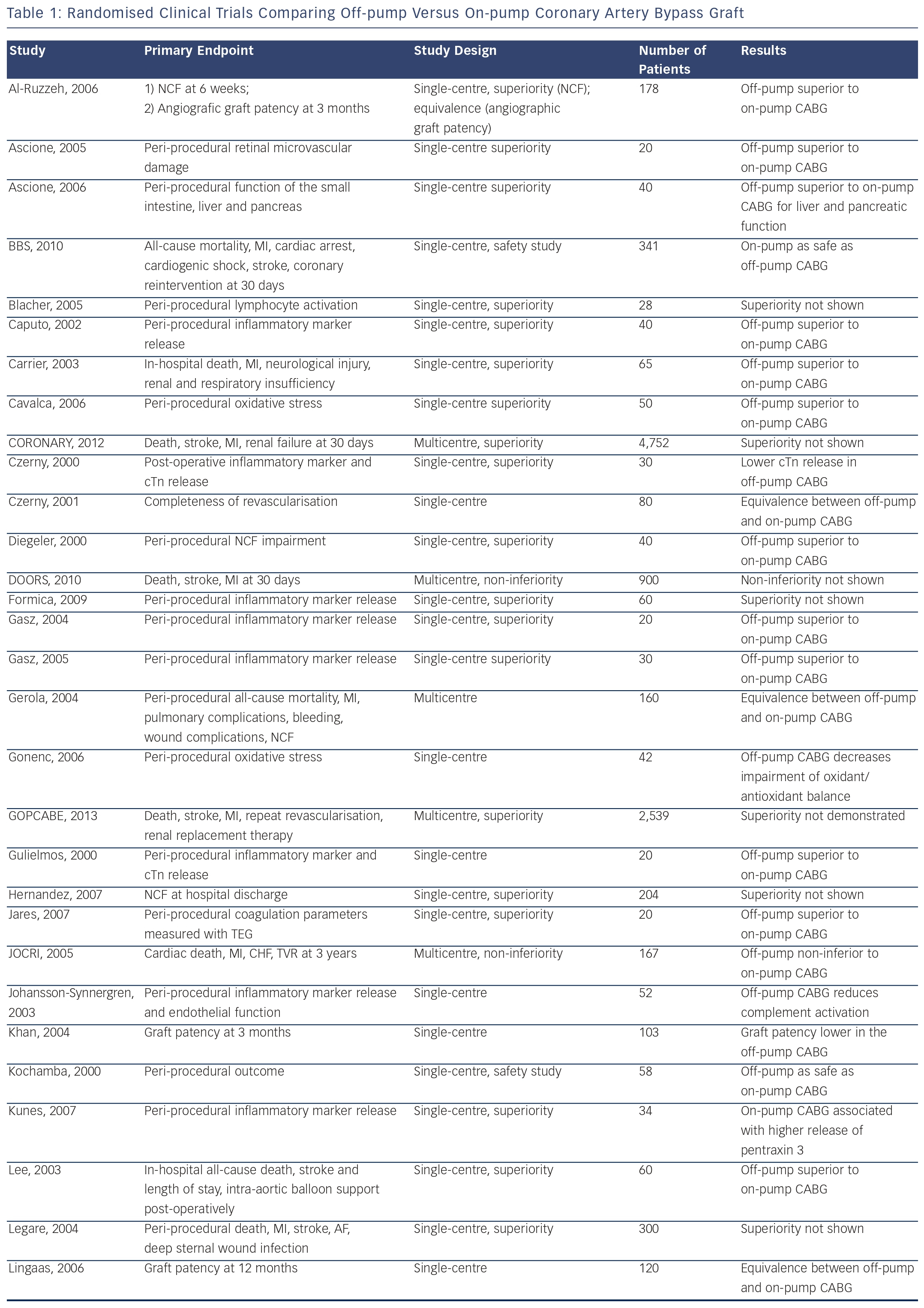
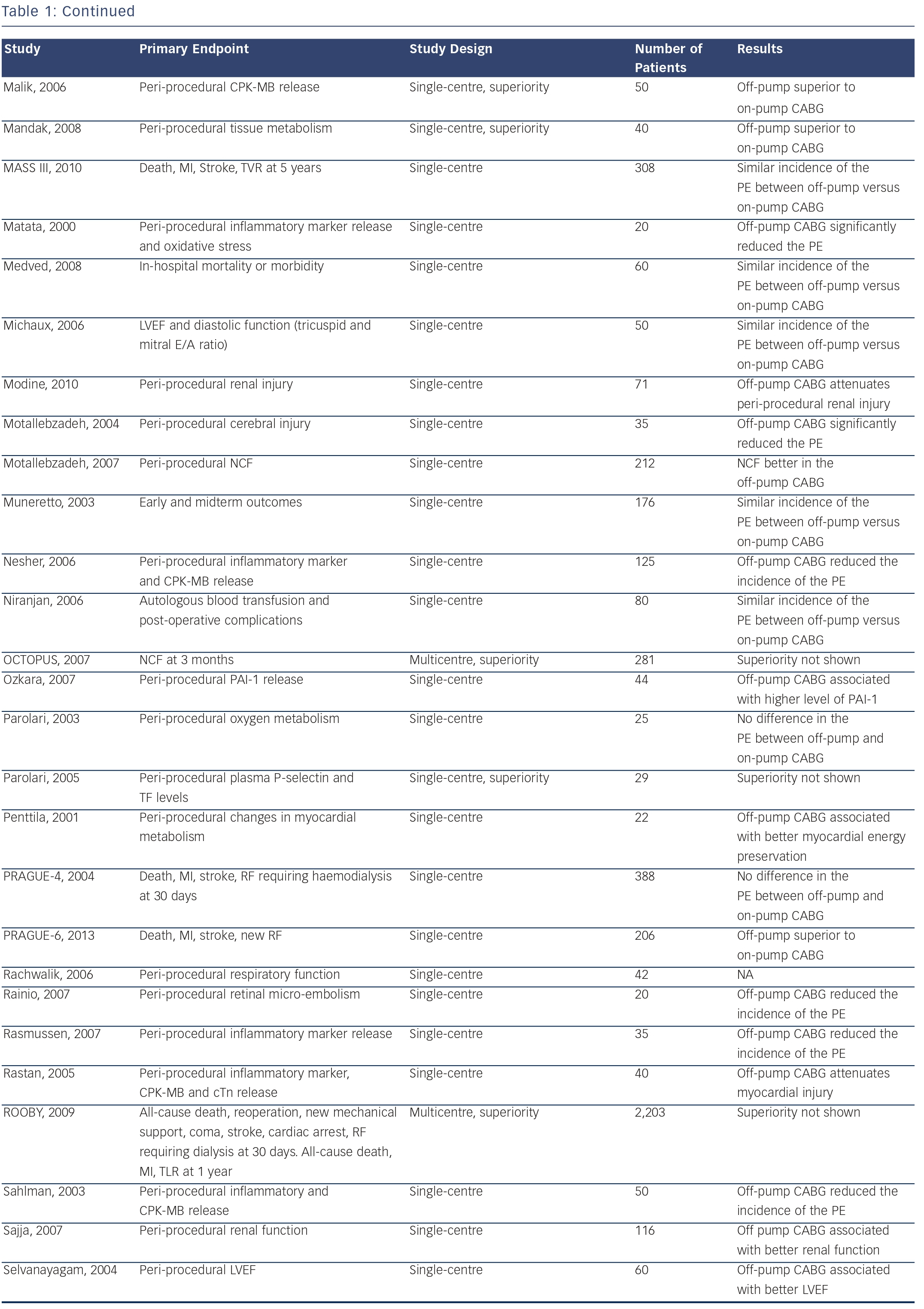
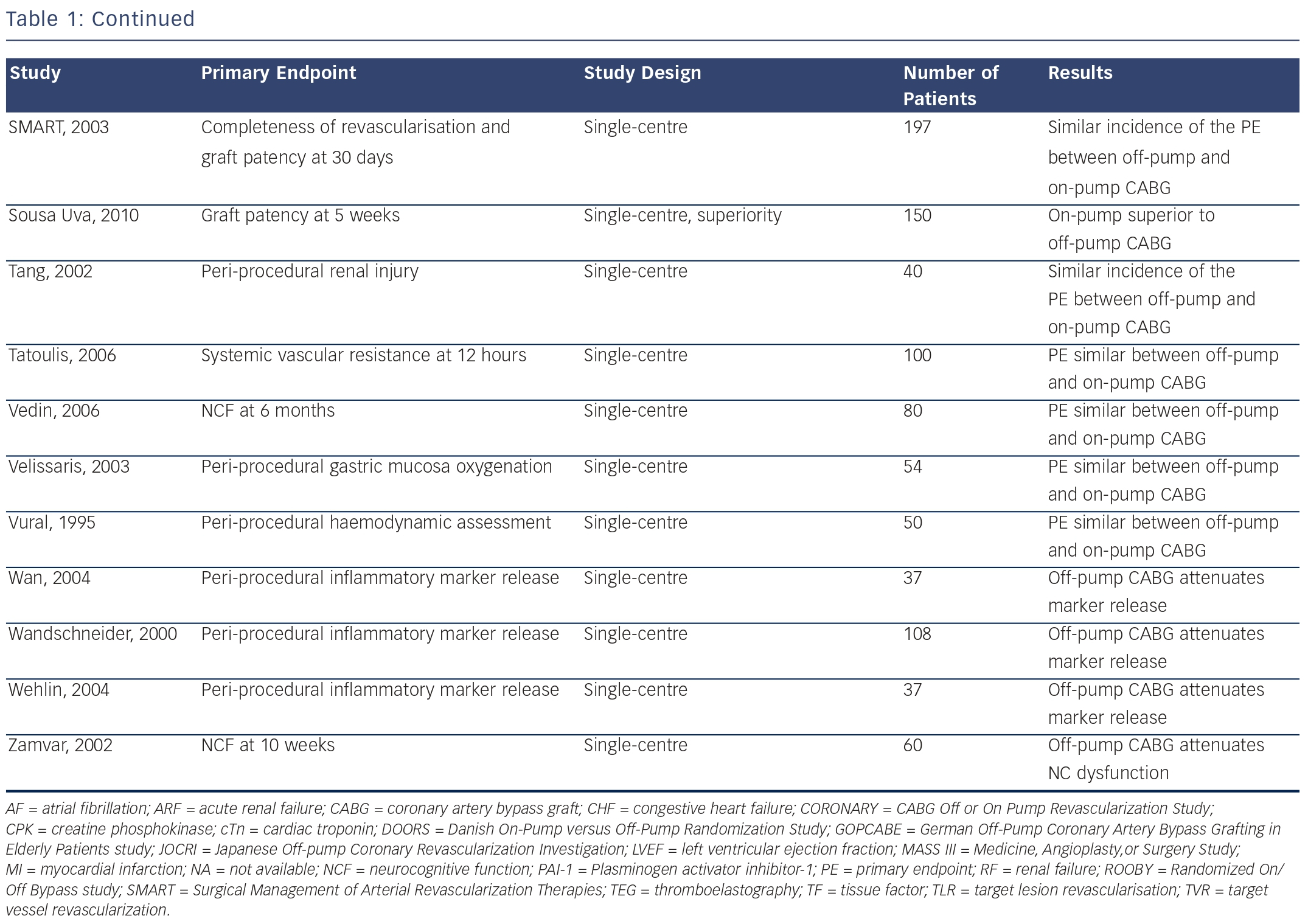
Specifically, in a propensity matched analysis involving more than 42,000 patients, there was a 35 % reduction in the risk of stroke in patients treated with off-pump CABG compared with those treated with on-pump CABG.27 In sharp contrast, in the recently published CABG Off or On Pump Revascularization Study (CORONARY), no significant difference in stroke rates was apparent between patients treated with on-pump CABG versus those treated with off-pump CABG. Similar results were apparent in two other recently published RCTs: German Off-Pump Coronary Artery Bypass Grafting in Elderly Patients (GOPCABE)28 trial and PRAGUE 6 trial.29 Several other RCTs comparing off-pump versus on-pump CABG have been performed, and results are summarised in Table 1.
In order to clarify relative safety and efficacy of off-pump versus on-pump CABG, several meta-analyses have been performed, but results have been controversial too. In particular, in the meta-analysis by Afilalo et al.,30 including 59 RCTs with 8,961 patients, there was a significantly lower 30-day risk of stroke with off-pump CABG compared with on-pump CABG. In sharp contrast, in the broader meta-analysis by Moller et al.,31 including 86 RCTs with 10,716 patients, there was no significant difference in the risk of stroke at long-term follow-up. Evaluation of different timepoints, study selection and different methodology likely explain discrepancies. It should be noted that neither of these two metaanalyses included the CORONARY trial, which with 4,752 patients enrolled, is the largest RCT performed to date.
In the largest meta-analysis performed to date, including the CORONARY trial and analysing the risk of stroke in 22,279 patients, Palmerini et al. showed that patients treated with off-pump CABG had a significantly lower 30-day risk of stroke than patients treated with on-pump CABG. However, when the analyses were restricted to high quality studies, studies with either >100 or >1,000 patients, or to studies with definition or adjudication of stroke by a clinical events committee, the precision of the point estimate was reduced, suggesting that the overall result may have been affected by studies with substantial risk of bias. Most notably, the odds ratio (95 % confidence interval [CI]) for stroke in trials of off-pump versus on-pump CABG enrolling >1,000 patients was 1.10 (0.67, 1.72).
These data therefore do not clearly support the hypothesis of a significant reduction in the risk of stroke with routine implementation of off-pump CABG compared with on-pump CABG. With an absolute risk reduction of 0.1 % and a relative risk reduction of 11.0 % with off-pump CABG versus on-pump CABG observed in the CORONARY trial, more than 300,000 patients would be necessary to assess whether off-pump CABG truly reduces the risk of stroke compared with on-pump CABG with test power of 80 % and alpha (α)=0.05.
Anaortic Off-pump Coronary Artery Bypass Graft Approaches
As discussed above, RCTs and meta-analyses do not consistently support the hypothesis that routine implementation of off-pump CABG might reduce the risk of stroke compared with on-pump CABG. However, the specific technique used to perform off-pump CABG in those RCTs has not been reported in detail.7 Off-pump CABG in fact encompasses a variety of surgical techniques that entails different levels of aortic manipulation, including partial or side clamping of the aorta, use of the HEARTSTRING® Proximal Seal System (MAQUET, San Jose, CA, US)32 and total arterial revascularisation without cross-clamping.
Partial clamping entails surgical manipulation, and does not eliminate the clamp-related risk of stroke. In sharp contrast, anaortic approaches avoids any clamping of the aorta during off-pump procedure by performing in situ grafting using both mammary arteries and/or T- or Y-grafting. Several studies have suggested that anaortic approaches may minimise the risk of stroke in patients undergoing CABG. In a meta-analysis including 12 observational studies, the anaortic approach was associated with a significant reduction in the risk of stroke compared with both conventional CABG and off-pump CABG with partial clamping.33 In addition, Halbersma et al. showed very low rates of stroke in a cohort of 400 consecutive patients undergoing off-pump CABG with anaortic approaches.34 When the results were analysed in the perspective of the surgical arm of the Synergy between percutaneous coronary intervention with Taxus and Cardiac Surgery (SYNTAX) trial,35 a clear trend was apparent, suggesting a reduction of the risk of stroke in patients treated with anaortic approaches compared with patients treated with conventional CABG (0.8 % in the study by Halbersma et al. versus 2.2 % in the surgical arm of the SYNTAX trial). Moreover, the 0.8 % risk of stroke associated with anaortic approaches34 closely matched the 0.6 % risk of stroke associated with stenting in the SYNTAX trial.35
Another device that can be used to minimise aortic manipulation is the HEARTSTRING seal. The HEARTSTRING seal is delivered at the site of circular aortotomy to avoid uncontrolled spurting of blood while the graft is sutured.32 After completion of the anastomosis and before tightening of the suture, the device is removed. In a propensity score matched analysis including 4,314 patients, Emmert at al. showed that the occurrence of stroke was significantly lower in patients treated with anaortic approaches using the HEARTSTRING device compared with patients treated with off-pump CABG using partial clamping.36 Moreover, the HEARTSTRING device had similar rates of stroke as total in situ arterial revascularisation, which avoids any touch of the aorta and therefore is considered the gold standard technique to minimise the risk of stroke.
Can We Minimise the Risk of Stroke After Coronary Artery Bypass Graft? Techniques and Patient Selection
Accurate risk stratification and careful selection of the strategy of revascularisation are key factors to minimise the risk of stroke. The presence of severe atherosclerotic disease of the ascending aorta may be associated with a stroke rate up to 45 % if no modifications in the operative technique are implemented.37 Depending on the individual risk profile of patients, several options can be considered to minimise the risk of stroke. If the risk of stroke appears prohibitive with CABG, and anaortic approaches cannot be used, PCI should be considered as an alternative. In case of severe atherosclerotic disease of the ascending aorta, off-pump CABG with anaortic approaches should be implemented. Total arterial revascularisation with in situ grafting using both mammary arteries and/or T- or Y-grafting should be considered the gold standard to minimise the risk of stroke.
When complete revascularisation cannot be achieved with total arterial revascularisation, use of the HEARTSTRING device may help in minimising aortic manipulation. Use of intra-operative epiaortic ultrasound, which can precisely characterise site and extension of atherosclerotic disease, may help the surgical decision-making approach. In the study by Bolotin et al., intra-operative findings of atherosclerotic disease of the ascending aorta with epiaortic ultrasound led to a change in the surgical strategy in 28 % of cases.10 Moreover, in cases in which on-pump CABG cannot be avoided, epiaortic ultrasound may help in identifying a relatively disease-free portion of the aorta to minimise the risk of atheroembolism when clamping or cannulating the aorta.
Despite some studies suggesting a potential benefit of anaortic approaches for high-risk patients, this technique has not been widely embraced. For several reasons, including the technical requirements for performing graft anastomoses with the beating heart and the concern for long-term patency, most surgeons worldwide still prefer to perform CABG with cardiopulmonary bypass.38 Thus, much of the evidence derived from the aforementioned studies has been contributed by highly experienced centres with surgeons that have developed high proficiency in performing off-pump CABG. Whether this technique can be safely extended to all cardiac surgical centres, remains to be determined.
Use of epiaortic filters has also been advocated as another possible strategy to minimise the risk of cerebral embolism in patients with severe atherosclerotic disease of the ascending aorta, who are not deemed suitable for anaortic approaches. The filter is inserted through a modified arterial cannula immediately before releasing the cross-clamp, and it remains in the aorta until cardiopulmonary bypass is discontinued. In a study involving 77 patients, implantation of the filters proved to be feasible, safe and uneventful.39 Particulate emboli were retrieved in 44 patients, the predominant origin of which was atheromatous. In a randomised trial including 1,289 patients, particulate emboli were detected in 598 (96.8 %) of 618 successfully deployed filters.40 In addition, a significant reduction in post-operative renal complications was apparent in patients in whom filters were implanted compared with the control group.
More controversial appears the management of patients with carotid artery disease that have to undergo CABG. The prevalence of severe carotid disease in this setting is around 6–12 %.41 Three approaches are commonly used: carotid endarterectomy followed by CABG, combined carotid endarterectomy and CABG, and more recently carotid stenting followed by CABG. In a propensity matched analysis of 350 patients in which these three approaches were compared, Shishehbor et al. showed significantly lower long-term rates of all-cause death, myocardial infarction and stroke in patients treated with carotid stenting followed by CABG in comparison with both carotid endarterectomy followed by CABG (adjusted hazard ratio [HR] 0.33, 95 % CI 0.15–0.77; p=0.01) and combined carotid endarterectomy and CABG (HR 0.35, 95 % CI 0.18–0.70).42 However, due to the observational nature of the study, these data should be considered hypothesis generating, and further randomised trials are warranted.
Optimal blood pressure management, prompt recognition and treatment of new onset atrial fibrillation, prevention of rewarming temperature >37°C,43 use of alpha-stat pH management44 and prevention of hyperglycaemia during surgery45 are other recommendations that should be considered depending on the individual risk profile of patients.
Conclusions
Notwithstanding the remarkable improvement in surgical, anaesthetic and medical management, the risk of stroke after CABG has not significantly declined. Risk stratification is of the utmost importance for identifying vulnerable patients. Specifically, pre-existing cerebrovascular disease and atherosclerosis of the ascending aorta are major determinants of the risk of peri-operative stroke, and should be always carefully scrutinised. RCTs and meta-analysis do not clearly support routine implementation of offpump CABG as a strategy to minimise the risk of stroke. Observational studies have suggested that anaortic approaches might reduce the risk of stroke compared with conventional CABG in patients with severe atherosclerosis of the ascending aorta. Further randomised controlled trials are warranted to confirm this hypothesis.