Transcatheter aortic valve implantation (TAVI) is a valuable treatment option for patients with severe symptomatic aortic stenosis.1 Its use is supported by the results of multiple randomised controlled trials (RCTs) exploring the entire surgical risk spectrum, including inoperable, high-risk, intermediate risk and low risk patients.2–8 TAVI is associated with a small but not negligible complication rate that exceeds that observed for percutaneous coronary intervention by approximately 10-fold and strongly impacts on overall morbidity, mortality and costs.9–12
Thrombotic events are a major concern during and after TAVI procedures and are associated with various factors, including procedure-related and valve-related factors.13,14 The typical TAVI population is highly comorbid and several coexisting conditions (e.g. AF) may enhance the individual’s risk of thrombosis.15 The multifactorial mechanism behind thrombotic events after TAVI suggests the need for adequate antithrombotic therapy, including antiplatelet and/or anticoagulant agents.16 However, the prescription of multiple antithrombotic drugs is not desirable in the older population that is currently offered TAVI, since any benefits may be outweighed by an increased propensity to bleed, which is a risk after TAVI irrespective of a patient’s background and adjunctive pharmacotherapy.11 Importantly, a large proportion of TAVI patients have comorbidities requiring long-term oral anticoagulation (OAC) or dual antiplatelet therapy (DAPT), which makes it difficult to balance the risks of ischaemia and bleeding for subsequent drug selection.13
Since the current evidence is not conclusive and recommendations are mostly supported by expert opinion, uncertainties about optimal antithrombotic therapy after TAVI remain.17 The purpose of this article is to critically explore the role of antithrombotic therapy after TAVI, focusing mainly on anticoagulant therapy and its connection with clinical and pathophysiological effects in patients with and without a long-term indication for OAC.
Complications of TAVI
Despite consistent improvements in patient and device selection, technical and procedural performance and clinical management, TAVI is still fraught with risk. Both thrombotic and bleeding complications may occur, which have a strong impact on early and long-term clinical outcomes.9
Thrombotic Events
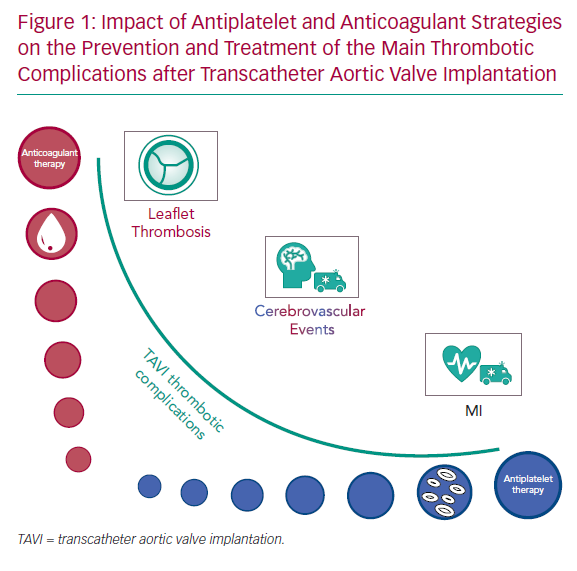
Definitions of thrombotic events following TAVI have been standardised by the Valve Academic Research Consortium (VARC) and updated VARC-2 consensus.18,19 Cerebrovascular events, AF and valve thrombosis account for the majority of thrombotic complications associated with TAVI and are the reason that antithrombotic therapy with antiplatelets and/or OAC is recommended (Figure 1).
High concentrations of tissue factor and thrombin surrounding degenerative aortic stenosis leaflets contribute to local inflammation and thrombogenicity. The exposure of diseased leaflets and irregular blood flow around the device strongly increase the periprocedural prothrombotic environment associated with TAVI.20 Thrombotic risk is also enhanced by coexisting conditions. Approximately 70% of TAVI patients suffer from coronary artery disease, which increases the risk of subsequent ischaemic events.2–8,21 Peripheral artery disease and extracranial carotid artery stenosis occur in 24–48% and 30% of patients, respectively.22,23 AF also plays a major role, as it has a detrimental impact on cardiovascular and cerebrovascular events (CVEs), mortality and length of hospitalisation and affects one-third of TAVI patients, presenting as a new-onset condition in about 36% of individuals.24–26
MI
MI is modestly frequent after TAVI, occurring in up to 5.1% of patients at 30 days, and has a detrimental impact on long-term outcomes.27 TAVI patients are usually screened for coronary artery disease and eventually treated, but whether complete revascularisation before TAVI reduces ischaemic events and improves clinical outcomes is still matter of debate. Current knowledge is based on small observational trials and their meta-analyses, therefore the evidence is of poor quality.28–32 Myocardial injury may also result from other causes, including tissue compression, hypoperfusion or direct cardiac injury in cases of transapical access.13
Cerebrovascular Events
CVEs are a major concern for TAVI patients and include VARC-2-defined stroke and transient ischaemic attack.19 Based on their timing, these events may be classified as acute (within 24 hours; about 50% of CVEs), subacute (1–30 days) and late (>30 days).33 It should be highlighted that the incidence of CVEs has remained substantially unchanged in recent decades, signalling the need for further improvements in this field. Across TAVI landmark studies, the 30-day stroke incidence ranges between 0.6% and 6.7%, increasing to 1.2–10.6% at 1 year.2–8,21
The mechanism underpinning CVEs following TAVI is multifactorial. It includes valve-related flow turbulence, vessel wall disruption, metallic frame exposure (which in turn induces platelet activation) and patient-related prothrombotic factors, irrespective of the valve type (balloon- or self-expandable) or procedural approach (transfemoral or transapical).34 Other patient-related factors, such as AF, periprocedural hypotension or hypoperfusion, should be considered determinants of CVEs.35 The acute events seem to be slightly different: thrombi derive from the interaction between the device and the calcified aortic valve, with debris dislodgment due to the placement of wires and catheters, pre- and post-dilatation.36,37
Interestingly, neuroimaging studies have demonstrated the appearance of silent cerebral lesions with embolic features following TAVI in up to two-thirds of patients.38,39 Their clinical and prognostic significance is still unknown and will probably be ascertained once TAVI is offered to a younger population. However, embolic cerebral protection devices are available and preliminary studies have demonstrated a reduction in total lesion burden without stroke or survival benefits.40,41
Leaflet Thrombosis
The European Society of Cardiology (ESC), European Association of Percutaneous Cardiovascular Interventions and European Association for Cardio-Thoracic Surgery published a joint consensus statement to standardise the definition of bioprosthetic valve dysfunction (BVD), an all-encompassing term including all factors underlying bioprosthesis failure.42 In this instance, bioprosthetic valve thrombosis refers to a spectrum of abnormalities ranging from minimal hypo-attenuating leaflet thickening (HALT) to clinically overt obstructive thrombosis.43,44
Epidemiological characteristics of this phenomenon are hard to assess because there is high heterogeneity in definitions and diagnostic imaging used in various studies.45 Two registries established a higher prevalence of leaflet thrombosis among TAVI patients compared to those undergoing surgical aortic valve replacement.46,47 Recently, the imaging sub-study of the Placement of AoRTic TraNscathetER Valves (PARTNER) 3 trial confirmed this finding. HALT was found to have an incidence of approximately 10% at 30 days, increasing up to 24% at 1 year.48 Interestingly, HALT minimally affects transvalvular gradients, does not cause clinical adverse events, and spontaneously resolves in half of cases without any need for OAC.48 A recent meta-analysis of one RCT and 17 observational trials found that, whereas clinically apparent thrombosis is very rare (0.48% per year), subclinical leaflet thrombosis is common (16.32% per year).49 Importantly, leaflet thrombosis seems to lead to an increased risk of further thrombotic events, probably due to the distal embolisation of microthrombi;49 unfortunately, current data are too sparse to draw a final conclusion.
Diagnosis of leaflet thrombosis is made based on haemodynamic (e.g. increased mean trans-prosthetic gradient, new/worsened intra-prosthetic regurgitation), imaging (leaflet thickening or reduced motion) and therapeutic ex juvantibus (improvement on anticoagulant therapy) criteria.42 The assumed pathophysiological mechanisms of leaflet thrombosis include reduced blood flow between the Valsalva sinuses and bioprosthetic leaflets, tissue fissuring, endothelium exposure and incomplete prosthesis expansion or apposition, which in turn delays the process of endothelisation.50,51 Several factors are independent predictors of leaflet thrombosis: body mass index >30 kg/m2, large valve diameter (>28 mm), balloon-expandable prostheses, valve-in-valve procedure and single antiplatelet therapy (SAPT) administration.52,53 Interestingly, in comparison with OAC, SAPT and DAPT are less effective on these thrombi in many cases because they develop in a low shear-stress setting that often involves thrombin-mediated processes rather than platelet aggregation (Figure 1).13
Knowledge of subclinical leaflet thrombosis is scarce and controversial but it seems to be a potential concern in relation to clinical outcomes and long-term valve durability.13,43 OAC has exhibited good efficacy in the prevention and treatment of subclinical and clinical leaflet thrombosis. However, since the association between subclinical leaflet thrombosis and clinical outcome is unclear, no recommendations can be made for routine pharmacological prevention.13 The imaging sub-study of the Medtronic Evolut Transcatheter Aortic Valve Replacement Low Risk Patients trial (NCT02701283) will further elucidate this topic.8
Bleeding Events
A major concern during and after TAVI is bleeding events. These are ranked in severity from minor to major and life-threatening according to the VARC-2 consensus scale19 and are more specifically defined by the Bleeding Academic Research Consortium.54 A rough but essential distinction exists on the basis of the bleeding site; there are two classes of events with different incidences, clinical features and prognostic implications, namely access-related and non-access-related bleeding.18,19,54 A further criterion, similar to CVEs, considers the timing of bleeds, which may be split into periprocedural, early (within the first month) and late.
Periprocedural bleeding mainly results from access-site complications arising from mechanical causes (e.g. large delivery sheaths in patients with peripheral artery disease and vascular calcifications) and may be predicted by several parameters, including sheath-to-femoral artery ratio and femoral artery calcium score.55,56 A small proportion of periprocedural bleeds is due to cardiac structural damage leading to pericardial tamponade, especially during surgical repair of the apex using the transapical approach.57 Late bleeds (>30 days) are mainly non-access-related and involve other systems (gastrointestinal, genitourinary, neurological).9 Access-site events occur almost entirely within the first month (periprocedural and early); whereas non-access-site bleeds have an initial peak and then continue to accrue over time.9
When assessing the characteristics of bleeding events, two limitations should be acknowledged. First, despite the efforts that have gone into producing consensus documents, the definitions of bleeds, timing of assessment and event adjudication are heterogeneous among TAVI trials and registries.18,19,54 Second, initial TAVI trials included older and frailer patients with a higher inherent bleeding risk, resulting in an increased event rate.58 Taking these aspects into account, life-threatening or major bleeding rates have been reported to be between 2.4% and 41.7% at 30 days and between 3.2% and 46.1% at 1-year follow-up.2–8,21 Notably, regardless of the aetiology, both acute and late bleeding are associated with poor clinical outcomes and increased mortality rate.9,10,12 In addition, bleeds may be augmented by coexisting conditions, such as older age, frailty, fall risk, renal failure, liver disease, malignancy, anaemia and coagulation disorders, as well as by AF and antithrombotic therapy.59–64 Finally, a periprocedural thrombo-inflammatory state and reduced platelet turnover in the older patient may act synergistically, resulting in transient thrombocytopenia in 69–87% of TAVI patients, signalling severe impairment of general homeostasis.65–67
Gastrointestinal bleeding associated with aortic stenosis is due to the shear stress and flow turbulence across the stenotic aortic valve, which may cause the cleavage of high-molecular-weight multimers of von Willebrand factor, a coagulation protein responsible for haemostasis. This condition, known as Heyde’s syndrome or acquired von Willebrand factor disease type 2A, prolongs the adenosine diphosphate closure time and leads to a tendency to bleed.68 Interestingly, this condition may also develop as a result of a moderate-to-severe paravalvular leak after TAVI, and a prolonged adenosine diphosphate closure time (>180 seconds) was shown to be predictive of significant aortic regurgitation and higher 1-year mortality rate following TAVI.69 The role of paravalvular leak as a surrogate predictor for bleeding tendency and mortality following TAVI is still unclear.70
Finally, strategies aiming to reduce the bleeding rate following TAVI include technological improvement, reduction in sheath size, optimal patient selection, choice of access route and the use of percutaneous closure devices. Increase in the operator’s experience also reduces the chances of bleeds following TAVI.
Antithrombotic Therapy Following TAVI
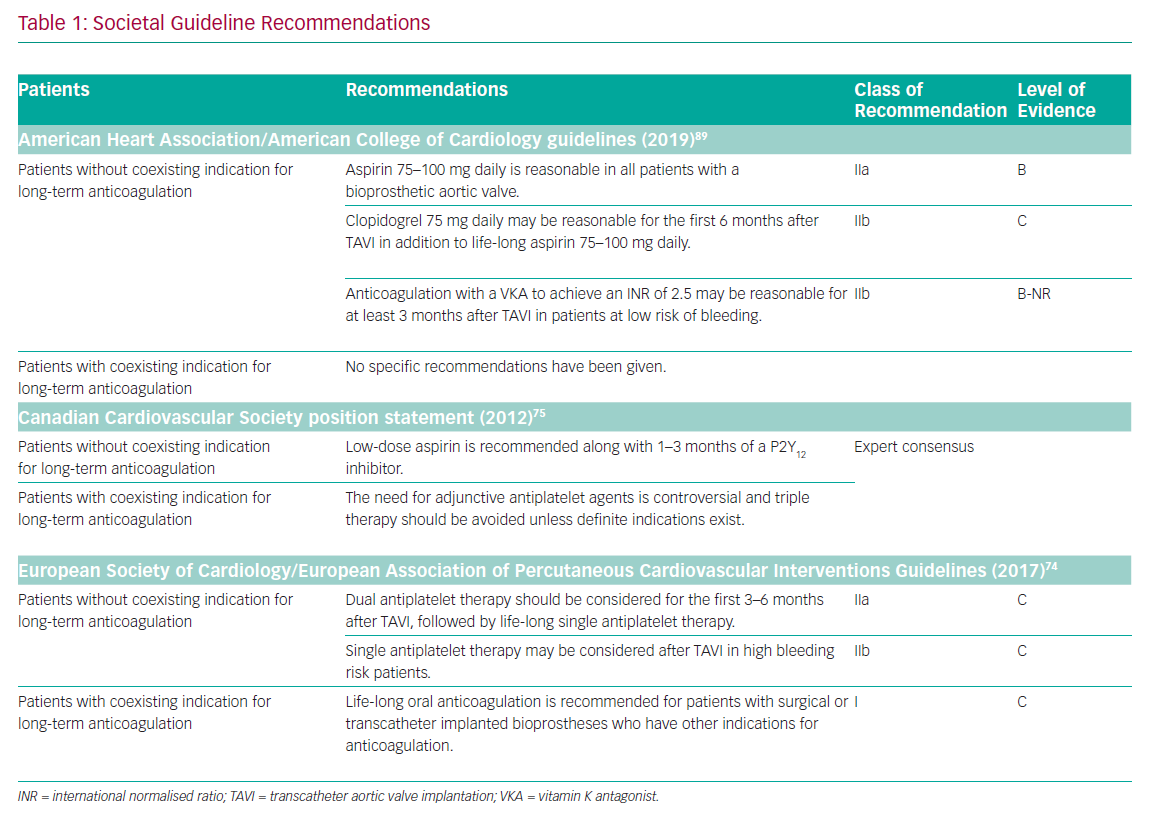
As larger RCTs are still awaited, current guidelines are based on observational studies and expert opinion (Table 1).71 The American Heart Association/American College of Cardiology guidelines recommend:
- life-long acetylsalicylic acid (ASA) (class IIa, level of evidence B);
- the consideration of DAPT with clopidogrel on top of ASA for the first 6 months (class IIb, level of evidence C); and
- the consideration of a vitamin K antagonist (VKA) with a target international normalised ratio of 2.5 in the first 3 months in patients at low bleeding risk (class IIb, level of evidence B).72,73
The attitude is slightly different on the other side of the Atlantic, where the ESC recommends lifelong SAPT after an initial DAPT for 3–6 months (class IIa, level of evidence C) and starting with SAPT as a more conservative option for high bleeding risk patients (class IIb, level of evidence C).74 Finally, lifelong OAC is recommended only for patients who have other indications for anticoagulation (class I, level of evidence C).74
The Canadian Cardiovascular Society recommends lifelong SAPT with ASA, preceded by a short 1–3 month course of DAPT.75 OAC should be reserved for patients with coexisting indications for long-term anticoagulation in which adding antiplatelet therapy is controversial. Interestingly, triple therapy is generally not recommended owing to the inherent high risk of bleeding in this population.75
Many of the societal guidelines do not issue specific recommendations for patients requiring long-term OAC, rendering this specific subgroup a residual field of uncertainty. Interestingly, a joint consensus document from the European Heart Rhythm Association and ESC Working Group on Thrombosis suggested that AF patients who undergo TAVI should receive OAC alone or a double therapy (OAC plus SAPT) if coronary artery disease coexists, or OAC alone if it does not.76 Unfortunately, OAC alone might not be enough to prevent stroke in such patients due to the various mechanisms underpinning thrombi formation, thus the dilemma continues.
Anticoagulant Therapy after Transcatheter Aortic Valve Implantation
The optimal antithrombotic strategy following TAVI is matter of debate. On the basis of the mechanisms surrounding thrombotic complications, both antiplatelet agents and OACs deserve consideration (Figure 1), with triple therapy representing a very questionable option.13,77 Up to two-thirds of patients currently receive a combination of OAC and antiplatelet therapy, but this seems to lead to a substantial increase in the composite of major or life-threatening bleeding.78 This practice is derived from analogy with percutaneous coronary intervention, considering the lack of high-grade guideline recommendations and the high prevalence of coronary or peripheral artery disease among TAVI patients.14
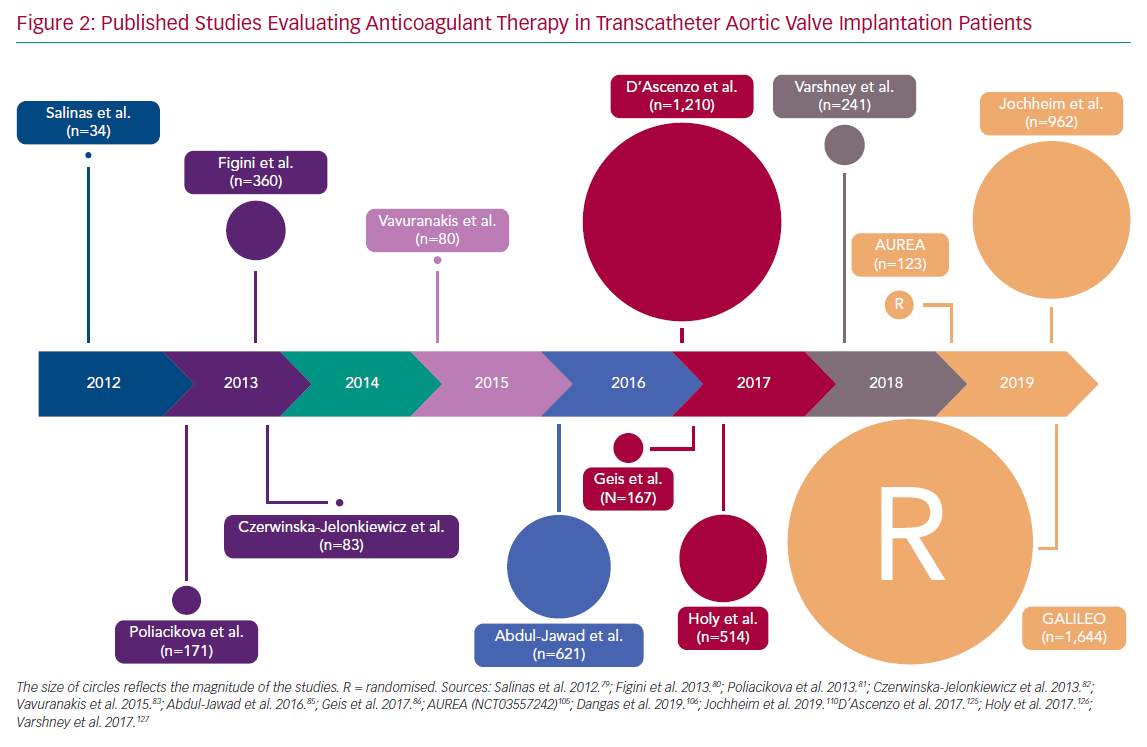
Current knowledge on OAC in patients who have undergone TAVI is largely confined to VKA and stems from observational trials (Figure 2).79–83 To assess this issue in a more careful and comprehensive way, it is useful to make specific considerations after splitting patients receiving TAVI into two groups, i.e. with and without a coexisting indication for OAC.
Patients with a Coexisting Indication for Anticoagulation
The most frequent indication for long-term anticoagulation is AF, followed by mechanical valve prostheses, deep vein thrombosis/pulmonary embolism, left ventricular thrombi, pulmonary hypertension or clotting disorders.84 How to treat these conditions after TAVI is an area of uncertainty and data from trials and registries are controversial.85–88 Importantly, when AF or other comorbidities require OAC, the antithrombotic regimen should rely on more specific recommendations.89
A large European and Canadian TAVI registry questioned the efficacy and safety of adding antiplatelet therapy to OAC: after a 13-month follow-up, there was no between-group difference in stroke, major cardiovascular events and death, while patients on dual or triple therapy experienced significantly more major or life-threatening bleeds.85 The large prospective FRANCE TAVI registry showed OAC at discharge to be an independent predictor of 3-year mortality;88 whereas a few observational studies have confirmed the safety and efficacy of OAC, either with VKA or a direct oral anticoagulant (DOAC).86,87
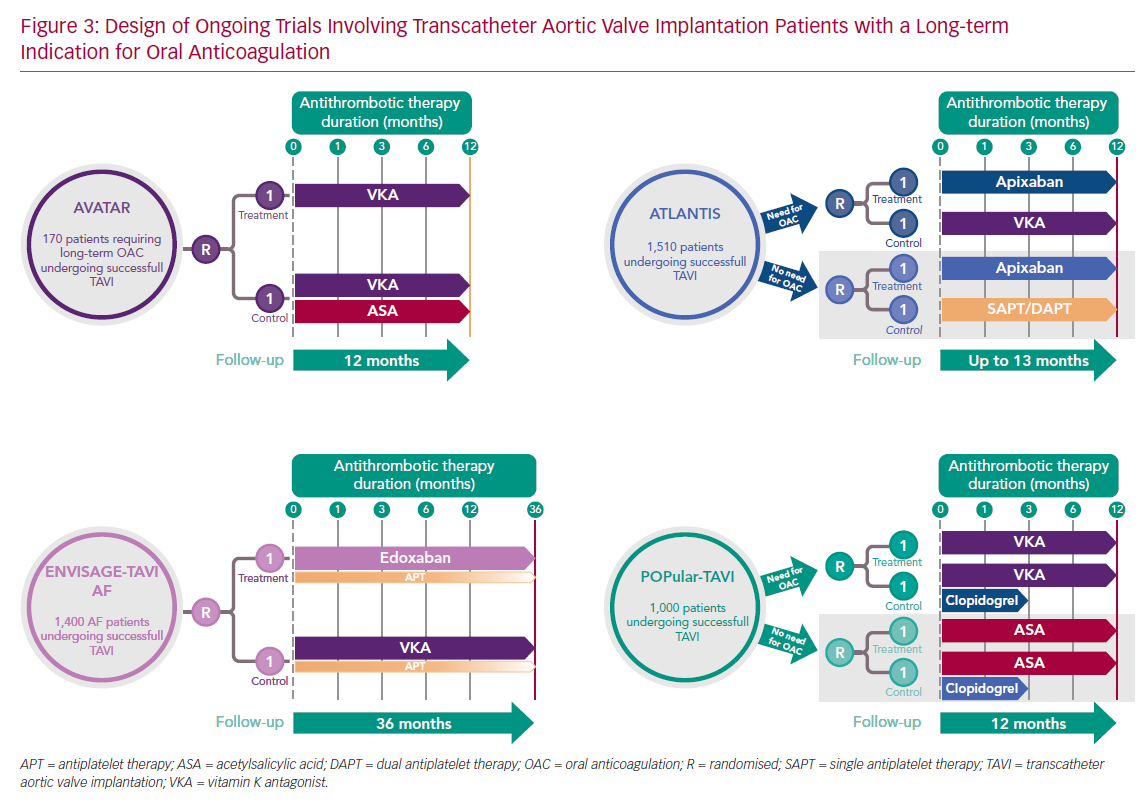
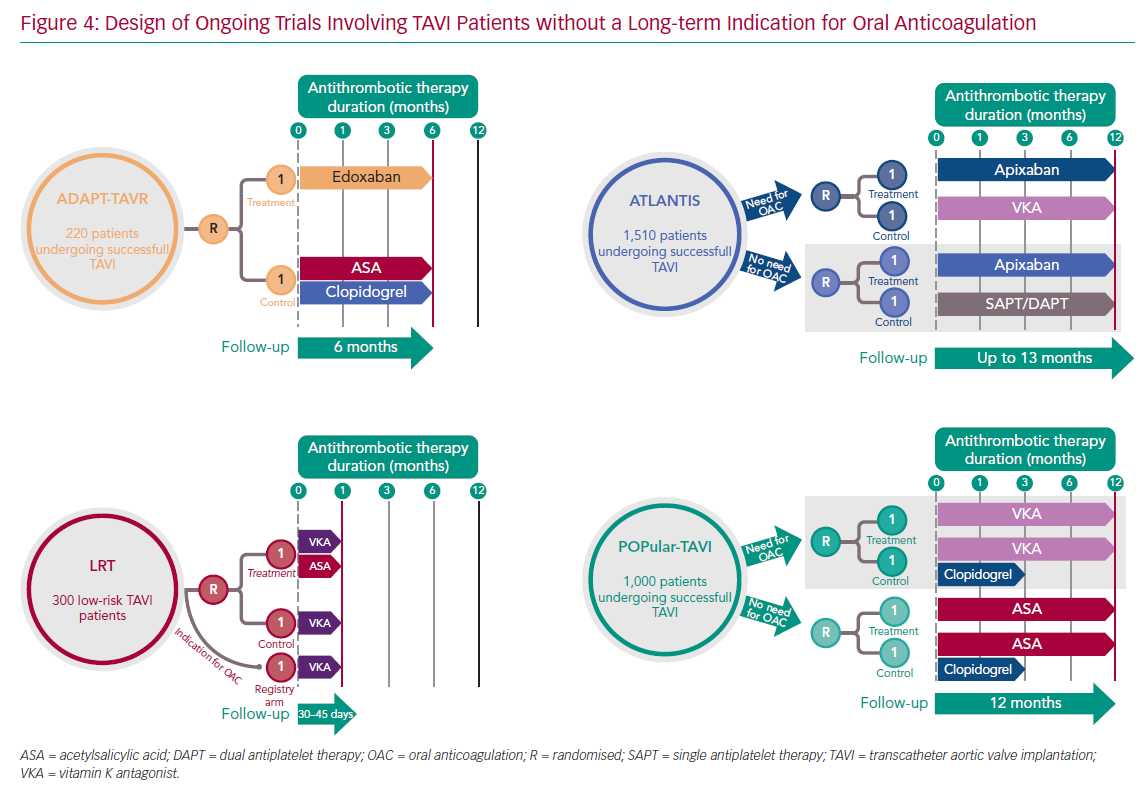
Further insights may come from ongoing investigations (Figures 3 and 4). The Antiplatelet Therapy for Patients Undergoing Transcatheter Aortic Valve Implantation (POPular-TAVI; NCT02247128) is a large multicentre open-label RCT questioning the value of adding 3 months of clopidogrel to single antithrombotic therapy (SAPT or OAC, as indicated) with respect to the co-primary endpoints of 1-year free from any or non-procedural bleeding; the results are expected in 2020.90,91
The multicentre open-label Clopidogrel Omission After Transcatheter Aortic Valve Replacement (CLOE) trial has a similar design to POPular-TAVI. It will enrol up to 4,000 TAVI patients to explore the role of routine clopidogrel (at least 6 months) on top of SAPT or OAC, as indicated, after TAVI to determine its effect on efficacy (composite of death, MI, stroke and valve thrombosis) and safety (major and life-threatening bleeding) endpoints.
The Anticoagulation Alone Versus Anticoagulation and Aspirin Following Transcatheter Aortic Valve Interventions (AVATAR; NCT02735902) trial is expected finish in April 2020.92 It has recruited TAVI patients with an underlying indication for long-term OAC and is investigating the 12-month net clinical benefit of OAC monotherapy with VKA or DOAC versus double therapy with aspirin plus OAC.
Edoxaban Compared to Standard Care After Heart Valve Replacement Using a Catheter in Patients With Atrial Fibrillation (ENVISAGE-TAVI AF; NCT02943785) is an open-label RCT enrolling up to 1,400 AF-TAVI patients and is comparing edoxaban 60 mg to VKA in terms of net adverse events and major bleeds up to 3-year follow-up. Notably, antiplatelet therapy – either SAPT or DAPT – may be administered at the investigator’s discretion in both the experimental and control arms. The final data are due to be collected in May 2020.93,94
The Anti-Thrombotic Strategy After Trans-Aortic Valve Implantation for Aortic Stenosis (ATLANTIS; NCT02664649) trial is a multicentre open-label RCT including 1,510 all-comers and is structured into two strata: the first comparing apixaban 5 mg to VKA in patients with indications for OAC; and the second evaluating apixaban 5 versus SAPT or DAPT in patients without the need for OAC. The primary endpoint is a composite of death, MI, stroke, systemic embolism, intracardiac or bioprosthetic thrombus, any episode of deep vein thrombosis or pulmonary embolism, or life-threatening or major bleeding at 12 months. The study results are expected to be published in 2020.95,96
Importantly, current considerations apply to contemporary (high-to-intermediate surgical risk) population and bioprostheses, needing a careful reappraisal of their external validity when TAVI will be offered to lower-risk and younger patients (with a subsequent decrease in CVE rates) and aortic bioprostheses will go through further improvements as expected.14
Patients without a Coexisting Indication for Anticoagulation
The use of anticoagulants following TAVI is based on a lesson from surgical valve replacement; however, while mechanical prostheses always necessitate long-term anticoagulation, this requirement has been overcome by modern bioprosthetic valves.97
While OAC is the standard of care for clinical or subclinical bioprosthetic leaflet thrombosis,49 its role in the prevention of stroke following TAVI is less clear. Although the prevailing mechanism of CVEs after TAVI is unknown, the rationale for using OAC relies on the knowledge that platelet activation and coagulation are highly interdependent and that thrombin plays a central role in both pathways.98 A recent analysis of the PARTNER 2 cohort strongly questioned the efficacy of OAC alone for preventing stroke after TAVI in these patients, showing that OAC without antiplatelets did not reduce the risk of stroke, probably due to platelet activation being triggered by the stent and increased thrombogenicity arising from endothelium exposure.99 Furthermore, antiplatelet therapy may disrupt the diffuse inflammatory and antithrombotic environment, acting as a substrate for stroke in patients with aortic stenosis.100
The FRANCE-TAVI registry has recently demonstrated the paradoxical effect of OAC monotherapy, which reduced BVD but independently increased the risk of death.88 A further consideration is that VKA may enhance the calcification of native and bioprosthetic leaflets, inhibiting a matrix vitamin K-dependent protein, thus leading to BVD.101 This represents an additional concern about the long-term use of VKA, whose benefit-to-risk ratio may worsen over time because the prevention of BVD becomes less relevant as time passes (BVD occurs mostly in the first 2 years) and bleeding risk increases with age.101
The Dual Antiplatelet Therapy Versus Oral Anticoagulation for a Short Time to Prevent Cerebral Embolism After TAVI (AUREA; NCT01642134) trial compared VKA to DAPT (ASA plus clopidogrel) in terms of new ischaemic and haemorrhagic cerebral lesions on 6-day and 3-month identified using diffusion-weighted magnetic resonance.102 No differences were noted between the two regimens with regards to new cerebral lesions or clinical events (death, stroke and major bleeding).103 It should be noted that the above results (PARTNER 2 sub-analysis, FRANCE-TAVI registry and AUREA) were obtained in the context of predominant VKA use, while the role of DOAC-based strategies is uncertain.104
Several RCTs exploring the role of OAC in TAVI patients who do not require it are ongoing (Figure 4). The randomised Strategies to Prevent Transcatheter Heart Valve Dysfunction in Low Risk Transcatheter Aortic Valve Replacement (LRT; NCT03557242) is exploring the add-on effect of VKA in low-risk TAVI patients taking ASA who have no reason for OAC administration, in terms of clinical outcomes and valve deterioration.105 The registry arm is implementing the same study design in patients requiring OAC.
The Global Study Comparing a rivAroxaban-based Antithrombotic Strategy to an antipLatelet-based Strategy After Transcatheter aortIc vaLve rEplacement to Optimize Clinical Outcomes (GALILEO) was the first to evaluate the role of a DOAC in TAVI patients not requiring OAC. This open-label trial randomised 1,644 patients to a DOAC-based strategy with long-term low-dose rivaroxaban 10 mg once daily (plus ASA for the first 3 months) or standard 3-month DAPT (ASA plus clopidogrel) followed by SAPT with ASA. The efficacy and safety outcomes were studied for both regimens.20,106 This trial was prematurely halted in August 2018 by the Data and Safety Monitoring Board due to safety concerns arising from an interim analysis as the rivaroxaban-based regimen had higher rates of thromboembolic events, bleeding and all-cause death.
Recently, the GALILEO-4D sub-study demonstrated that dual pathway inhibition (rivaroxaban 10 mg plus ASA) is more effective than DAPT (ASA plus clopidogrel) in preventing subclinical leaflet abnormalities as documented using 4D CT.107 However, these results should be cautiously interpreted due to the higher risk of adverse outcomes found with the rivaroxaban-based strategy in the parental trial.
Finally, among 220 patients otherwise not requiring OAC, the open-label Anticoagulant Versus Dual Antiplatelet Therapy for Preventing Leaflet Thrombosis and Cerebral Embolization After Transcatheter Aortic Valve Replacement (ADAPT-TAVR; NCT03284827) trial is comparing the effects of 6 months of edoxaban to DAPT with ASA plus clopidogrel on leaflet thrombosis assessed by 4D CT.108 The results are expected in December 2020.
In conclusion, while European guidelines did not provide specific recommendations supporting anticoagulant pathways in patients without a coexisting indication for OAC, American guidelines were published at a time when new evidence from large registries and the AUREA and GALILEO trials that showed a definite increase in the bleeding rate without significant benefits with OAC, was not available.
If Using an Anticoagulant, Which One is Best?
Since numerous concerns about OAC seem to derive from the prevailing use of VKA, several investigations have compared DOAC to VKA in terms of efficacy and safety among TAVI patients.87,109,110 Previous studies had rendered controversial results, probably due to the lack of randomisation and the small sample sizes. A recent multicentre non-randomised registry of TAVI patients requiring OAC compared a DOAC-based strategy (mostly rivaroxaban or apixaban) to a standard VKA strategy. While there was no difference in 30-day efficacy and safety outcomes (except a higher rate of non-disabling stroke with DOAC), the DOAC group had an increased rate of the 1-year composite endpoint of all-cause death, any stroke or MI without a corresponding decrease in bleeding. This is striking, because OAC was indicated for the prevention of AF-related stroke, for which DOAC are superior to VKA.111,112 Similar worries arose from the GALILEO trial, which was prematurely halted due to DOAC-related safety concerns.106 In spite of a clear superiority of DOAC over VKA for stroke prevention in the AF population, their administration to TAVI patients is currently not supported by strong evidence and the choice of the OAC regimen, if any, is empirical.
Special Subsets
The subject of antithrombotic therapy following TAVI may be more challenging than usual in certain subgroups who present other indications for antithrombotic drugs or display specific features influencing the ischaemia-to-bleeding risk trade-off.13 All demographic (age, gender, race), clinical (comorbidities) and procedural (technical skills and requirements) characteristics should be taken into account when dealing with this issue.113–116 Notably, several strategies could be applied to reduce the predominant risk profile in an individual patient, for instance the assessment of on-treatment platelet reactivity to tailor antithrombotic therapy to a patient’s response.117
Patients Requiring Antiplatelet Therapy after Transcatheter Aortic Valve Implantation
The main independent indication for antiplatelet therapy is chronic coronary syndrome, which affects up to 40% of TAVI patients, followed by acute coronary syndrome, peripheral artery disease and large aortic arch atheroma.118–120 In these patients, routine administration of OAC should be avoided. In the most complex scenario of patients in whom the absolute indications for antiplatelets and OAC merge, the matter becomes convoluted. As a rule, in AF patients with chronic coronary syndrome or peripheral artery disease the addition of antiplatelets to OAC should be discouraged, since this strategy does not appear to reduce the risk of ischaemic events but significantly increases bleeding risk.121,122 The AVATAR trial and the OAC subgroups of the POPular-TAVI and CLOE trials will provide some answers on the benefit-to-risk ratio of combination therapy including antiplatelets and OACs in patients undergoing TAVI.14,90,92
Patients at High Bleeding Risk: When Less is More
The management of this subgroup is very perplexing, since the adverse effects of antithrombotic drugs can easily overcome the intended benefits. Only ESC yielded a specific recommendation for this cohort, suggesting a SAPT (class IIb, level of evidence C).74 A typical high bleeding risk setting is outlined by the need for triple antithrombotic therapy (e.g. an AF patient who experiences acute coronary syndrome):123 importantly, since the primary aim is to reduce the adjunctive bleeding risk from antithrombotic drugs, left atrial appendage occlusion may be a valuable option. This is currently being evaluated among high bleeding risk TAVI patients.124 Importantly, this choice may represent more than an alternative to OAC, even in AF patients who have previously experienced major or life-threatening bleeding or an ischaemic stroke while on OAC.120
Conclusion
OAC is currently the standard treatment for leaflet thrombosis and represents a valuable option for ischaemia prevention among TAVI patients. However, all antithrombotic therapies should be weighted according to a patient’s thrombotic and bleeding risk profiles and comorbidities.
Current evidence is from the high- to intermediate-risk TAVI population, which is expected to significantly change in the next few years. The treatment of younger and healthier patients will soon reduce the burden of complications and the net benefit of antithrombotic regimens will likely vary accordingly.
Two questions remain unanswered: 1) what is the best antithrombotic regimen and duration in TAVI patients; and 2) are DOACs non-inferior or superior to standard VKA? Ongoing investigations will hopefully answer these questions. Taking into account further changes in typical TAVI populations and technological advancement, early and long-term antithrombotic regimens will need to be investigated in head-to-head studies and treatment options adapted to the individual patient’s needs, values and risk profiles.