Further to the statement that was released to members of the British Cardiovascular Intervention Society (BCIS) on 17 March 2020 about the coronavirus disease 2019 (COVID-19) pandemic,1 I have now been offered this opportunity to expand and update on the advice and comments in that original document in the light of recent developments, particularly with regard to personal protective equipment (PPE) and our recent guidance about cath lab procedures.
Members of the BCIS, along with their colleagues and patients, are facing the COVID-19 pandemic in an atmosphere of unparalleled stress and uncertainty about how we will be able to maintain the highest standards of clinical care.
As a group, our reaction to the challenges thrown at us by COVID-19 needs to be reasoned, calm, positive and energetic.
As before, the hottest issues remain:
- What is the appropriate nature and application of PPE?
- Are there some categories of patient who should not be offered treatment that we would normally consider (e.g. out of hospital cardiac arrest ventilated patients) or who should be offered alternatives (e.g. thrombolysis instead of primary percutaneous coronary intervention [PCI] for ST-elevation MI [STEMI]) to preserve cath lab access?
- What happens if a cath lab loses the ability to provide emergency cover?
It remains inappropriate for BCIS to attempt to provide proscriptive universal guidance concerning these and other contentious issues, for a number of reasons.
Firstly, there are a number of policies already laid down at a national level by NHS England, Public Health England (PHE) and the Department of Health, and by individual Trusts. Secondly, our understanding of the effects of this pandemic is evolving in a dynamic fashion, and there are significant differences in local Trust resources and logistical factors which may well shape the development of local policies. Finally, in some areas, particularly PPE, individual operators and centres have rapidly formed very strong views about the best algorithms for protecting staff and patients, many of which are incompatible, but which are considered non-negotiable. I will address this issue in detail below, in the light of recent PHE updated guidelines about general PPE, and the statement about specific cardiology procedures that was released a few days ago by the presidents of the British Cardiovascular Society (BCS), BCIS and the Heart Rhythm Society (HRS), and which are endorsed by PHE and the chief medical officers.
Clinical Decisions and Choice of Case Management
The presidents of BCS and BCIS have released a joint statement of support and advice to our members, and have contributed to an NHS England statement about recommendations for ongoing cardiology activities.2,3 Consistent with these guidelines, BCIS recommends that all our members follow some general principles, outlined here.
- Members should adopt, and comply with, national and local policies for testing, self-isolation and PPE compliance (see below).
- Members should develop local plans for possible scenarios in which their cath lab cannot provide emergency cover, whether due to staff absence or inadequate facilities/resources. We suggest that clinical leads/senior cath lab staff have discussions across local networks regarding potential cross cover for emergency patients between local centres, in case this becomes necessary.
- Be cautious about the implications of changing treatment pathways as a reflex response to this crisis. To this end, the NHS England guidance continues to recommend primary PCI for STEMI and angiography with a view to revascularisation for all non-ST-elevation MI (NSTEMI) patients, except perhaps the lowest risk group. This advice is based upon the assumption that the access to the cath lab and its specialised staff will remain stable. Clearly, in circumstances in which lab access is compromised by staff shortage or case load, hard alternative choices will need to be made. But the fact is that primary PCI for STEMI is associated with the best outcome for these patients, with the lowest mortality, fewest complication rates and shortest hospital stay. The same is true of a high-risk NSTEMI case. Making a rapid diagnosis using angiography and providing effective revascularisation, as appropriate, is again associated with a shorter admission, with a much lower reinfarction and subsequent revascularisation rate. By contrast, deferring NSTEMI patients may simply be deferring subsequent acute events and requirement for revascularisation. Having said that, the threshold for accepting patients for these procedures may have to change. This is going to be a matter of skill and judgement by experienced interventional cardiologists. The very elderly and comorbid patient cohort may not be included in this type of cath lab activity, given their increased risks and lower likelihood of benefit. Two examples highlight these points:
- Providing thrombolysis may seem like a good way of reducing demand upon cath labs, but what happens to the 25% of such patients who do not reperfuse? They then represent a major, and delayed, emergency dilemma. Even those patients who are successfully thrombolysed have a mandate to undergo angiography with or without revascularisation within 24 hours, according to international guidelines. The average length of stay for a primary PCI patient will be less than for a thrombolysed patient, given the higher likelihood of complications, and this may well lead to a higher overall exposure of NHS staff to the patient.
- Not offering emergency angiography to ventilated out of hospital cardiac arrest patients with ST elevation. Consider the 45-year-old who has cardiac arrest at the gym – it is unlikely that most of us would not want to offer cath lab access to them, so make such blanket policies only with great care. Therefore, we recommend a case-by-case approach.
- Members should reconsider the appropriate balance between PCI and coronary artery bypass grafting, as well as transcatheter aortic valve implantation (TAVI) versus surgical aortic valve replacement. As the NHS England document recommends, limited access to operating theatres and intensive care beds should push our balance of decision-making towards PCI and TAVI, respectively. This can still be based upon sound and considered decision-making processes involving discussion with colleagues and assessment of all available options. Unfortunately, we all need to remember that the option of ‘no intervention’ will necessarily become an important and useful one in our armoury during this crisis.
- Members should continue to provide clinical expertise, skilful judgement, calm leadership and dignified assurance.3
Personal Protective Equipment
The early variation in practices around the UK for PPE at all stages of patient contact was pretty alarming at the beginning of this crisis, but is becoming more uniform as NHS England catches up with the rapid spread of the virus and lessons learned from other countries. All patient exposure should now be associated with some form of PPE according to the latest national advice, a policy welcomed almost universally.
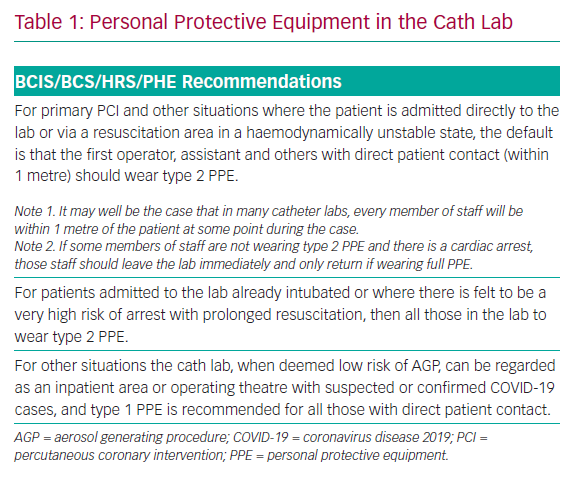
However, for BCIS members, it is the optimal PPE for cath lab procedures, especially primary PCI for STEMI, that has raised most anxiety and contention. I have been involved with Simon Ray (BCS President), Alistair Slade (President Elect, HRS) and Nick Linker (National Clinical Director for Heart Disease) and a number of others around the UK, with the aim of providing some definitive recommendations about optimal PPE for such cases. These recommendations were released a few days ago,4 and have been endorsed by NHS England and PHE, as being complementary to their recent updated general PPE guidance. I am pleased to reproduce the important part of this cath lab PPE guidance here. Our recommendations are shown in Table 1.
This guidance adopts an approach in which the PPE strategy is dependent upon both (a) the location in which patient contact occurs and (b) the likelihood that the contact will involve an aerosol generating procedure (AGP).
For cardiology this applies to any procedure requiring or likely to require resuscitation for cardiac arrest involving CPR ± intubation and to transoesophageal echocardiography. These procedures require disposable gloves, fluid resistant gowns, a filtering face piece respirator and eye/face protection wherever they are performed (termed type 2 PPE). Other procedures require disposable gloves, plastic apron (when not scrubbed), fluid resistant surgical mask and eye protection (termed type 1 PPE).
Ward environments are covered within the PHE guidance.
For cath lab procedures the PHE guidance can be applied to the individual case by the assessment of the senior clinician, together with senior cath lab staff, taking into account (a) the likelihood that the patient has the virus and (b) the chance the procedure will be AGP.
Conclusion
We will all continue to face the challenges offered up to us by this pandemic in a professional and dignified manner. Colleagues must be allowed choice and judgement in circumstances when so much of what we are being asked to decide upon comes down to individual interpretation and analysis of scant data.
Furthermore, our decisions about a clinical scenario on any given day may need to be modified by the rapidly changing nature of this outbreak in our individual centres.
I wish all BCIS members the strongest personal support on behalf of myself and the members of BCIS Council.