Heart failure is an epidemic in the US, affecting over 6 million people annually, and expected to surpass 10 million within a decade.1 Of patients with heart failure, approximately 10% progress to advanced heart failure, and patients with disease refractory to medication have high mortality rates of 30–50% within 1 year. The most effective treatment for advanced heart failure patients is a heart transplant, which has survival rates of >50% over 10 years.
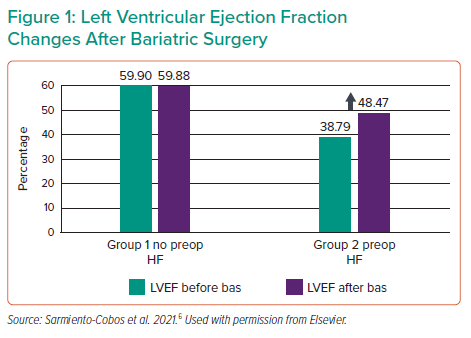
One of the factors that can influence heart health and failure is excess body weight. Research on obesity indicates that it can influence metabolic, hormonal and inflammatory systems, which, in turn, can influence cardiac health.2 Indeed, obesity correlates with increased risk of heart failure and has been rising steadily in the US, creating a need for better understanding and tools to treat obese heart failure patients.3,4 Bariatric surgery offers benefits for obese patients such as improved cardiovascular risk factors, lipid and inflammatory profiles and left ventricular (LV) function. However, bariatric surgery in heart failure patients results in a marked increase in in-hospital mortality and in-hospital complications, including MI, sepsis and kidney failure.5 Furthermore, heart transplant outcomes are bleak in obese patients, with increasing BMI correlating with increased 1-year mortality rates.6
More recently, the use of LV assist devices (LVAD) has shifted to a destination therapy, particularly in obese patients. As such, these patients represent an underserved population that requires innovative techniques to provide better treatment and outcomes. Dr Brozzi presented two clinical cases of morbidly obese patients with heart failure who were treated with off-label Impella use. The first patient progressed from repeated ventricular arrhythmia to cardiac shock, and was initially stabilised with intra-aortic balloon pumping (IABP), diuretics and IV milrinone. Implantation of an LVAD was not an option due to the risk of complications and patient lifestyle, and therefore an Impella CP was implanted instead, followed by a laparoscopic sleeve gastrectomy 24 hours later. The patient was stable throughout the surgery, with an unremarkable postoperative recovery. Within 2 months the patient had lost ~49 kg (108 lb), and was listed for heart transplant.
The second patient presented with acute heart failure due to non-ischaemic cardiomyopathy. This patient was also stabilised with IABP, diuretics and IV milrinone, and was also declined LVAD support due to potential complications. Instead, an Impella 5.5 was implanted before the patient underwent a laparoscopic sleeve gastrectomy. The patient was stable throughout the surgery with robust haemodynamics; again, patient recovery was unremarkable. The patient lost ~39 kg (85 lb) within 6 weeks and was listed on the heart transplant list. The patient was readmitted 75 days later with cardiogenic shock and was supported with venoarterial extracorporeal membrane oxygenation, but received a heart transplant 8 days later. Ultimately, the patient survived and was stable 3 months after transplant with a BMI of 35.5 kg/m2.
Dr Brozzi concludes that these cases demonstrate that bariatric surgery supported with transvalvular axial flow pumps is a feasible alternative to expedite weight loss and the heart transplant listing of severely obese patients with advanced heart failure.