More than 31,000 people were treated by emergency services following an out-of-hospital cardiac arrest (OHCA) in England in 2020; of these, just over 8% were successfully resuscitated and discharged alive from hospital. This is in line with comparable data from other European countries, and despite progress in access to basic life support training, public-access defibrillators and post-OHCA care, survival rates have remained largely unchanged.1,2,3
Although only a small percentage (<10%) of OHCA sufferers discharged alive from hospital experience a poor neurological outcome (defined as a Cerebral Performance Scale of ≥3), all survivors are at risk of experiencing long-term difficulties in their physical, cognitive and psychosocial recovery.4,5 Fatigue, cognitive impairment, anxiety/depression and difficulties in returning to normal day-to-day activities have all been documented, with different rates of prevalence reported across studies, possibly due to study methodology, sample characteristics and different time-points at which survivors have been followed up.6–8 There is an acknowledgement that survivors may have different support and information needs at different stages of their recovery process.5
A follow-up appointment tailored to this patient population is recommended by European Resuscitation Council (ERC) and American Heart Association (AHA) guidelines.9,10 Both guidelines identify the need for a multi-dimensional assessment covering physical and non-physical domains as well as provision of appropriate information. They also highlight the importance of a follow-up appointment inclusive of family members or ‘co-survivors’ who may well have their own psychological and information needs. In this context, we broadly define ‘co-survivor’ as a family member, spouse, partner or friend who provides support from admission to hospital through rehabilitation/recovery and beyond.
In 2017, a national framework for OHCA in England, Resuscitation to Recovery set out a range of recommendations to improve care after OHCA that included appropriate cardiac rehabilitation services after discharge.11 There are currently no common standards for a dedicated follow-up pathway after OHCA in the UK, and little is known around current practice. A survey with this goal was recently conducted by the Resuscitation Council UK in 2021 but has not yet been reported.12 It is currently unclear to what extent these appointments are offered routinely to all survivors and it is likely that there is substantial unwarranted variation across the UK. There is an urgent need to standardise services to improve care for these patients addressing several areas. These include referral criteria, optimal timing after discharge, which professionals lead the clinic with adequate access to an appropriate skill mix from a multi-disciplinary team (MDT), topics to be covered and what assessment tools are used, invitation of family members, how these follow-up clinics fit in with existing pathways of care and how they can contribute to signpost patients, and whether they are designed with patient and family input. It is also currently unclear if these services improve outcomes.
This document focuses on OHCA survivors with a favourable neurological outcome; it aims to provide a summary of the current guidelines on follow-up after OHCA and to suggest a set of essential and desirable actions to be taken, with patients’ expectations in mind to achieve best standards.
The Scale of the Problem: Significant Rehabilitation Needs for the Post-OHCA Patient
Post-OHCA Cognitive, Psychological and Physical Deficits Are Common
OHCA patients, in addition to more routine issues observed in the non-arrested cardiac patient, also exhibit a range of complex overlapping issues including physical, cognitive and emotional pathologies that have traditionally been challenging to address in conventional pathways of care. Nevertheless, identification of patients who develop cognitive impairment and/or affective/psychological disorders after cardiac arrest, the cost to patients and co-survivors of surviving a cardiac arrest and which treatments might promote recovery have all been reported as key gaps in current knowledge.10,13
Cognition
Cognitive deficits are very common in the early stages after surviving OHCA. Executive functioning has been identified as a domain particularly affected before discharge and in the first 2 weeks after OHCA together with memory and attention, with some evidence of improvement over time.14–19 Limited reporting of early cognitive deficits and possible intervention plans is therefore surprising considering cognitive impairment is subjectively reported by many OHCA survivors and objectively identified 6–12 months after the OHCA.7,20–22 Furthermore, cognitive impairment is a predictive variable of return to work and participation in society and – when identified early – has the potential to be treated with simple and cost-effective treatments.23,24
Psychological Distress
Psychological outcomes after OHCA have received increased attention in recent years, with a greater focus on the issue of survivorship and increasing recognition that co-survivors – close relatives and bystanders – may also have unmet needs.10,25,26 High rates of psychological distress (anxiety, depression and post-traumatic stress symptoms) are reported in several studies for survivors following OHCA.8 These can be persistent but tend to be most severe in the first few weeks post-arrest and tend to correlate with other quality-of-life measures.20,27 Around one-third of co-survivors have also been found to score highly on measures of post-traumatic stress symptoms around 2 years after the cardiac arrest, with those witnessing the arrest being most at risk, highlighting a current area of unmet need.28,29 Hence, timely access to psychological support is identified as a priority by both survivors and their family members.30
Physical Problems
Although physical deficits after cardiac arrest have received limited attention, problems with mobility, physical health and physical function are not uncommon.20,31 Fatigue is also a significant long-term issue for many survivors, and a barrier to return to work.32 Self-reported mobility problems, cognitive impairment and depression have all been found to be predictors for reduced participation in society.23
Cardiovascular and Genetic Factors
OHCA is often the index presenting event for significant underlying structural, ischaemic or pro-arrhythmic heart disease and hence survivors are usually investigated thoroughly as an in-patient for a definitive diagnosis and subsequent treatment.33 While at least 50% of cases are thought to be because of coronary artery disease, genetic causes such as cardiomyopathy or channelopathy are also highly prevalent, particularly in younger patients.34 After discharge and in the recovery period after the event, the presence of underlying conditions, associated symptoms and onward referral for investigation of and counselling for genetic causes, where appropriate, should be considered.35
Current Follow-up Standards and Programmes
Current follow-up guidelines in Europe recommend provision of information, screening of cognition and mood and referral to specialist services where appropriate.9 They also suggest a timeframe for follow-up (within 3 months of hospital discharge), to include fatigue as an area in need of assessment, specify that provision of information should not be limited to medical matters and specifically mention monitoring the wellbeing of family members as an integral part of the follow-up process. Pre-hospital discharge assessment of ‘physical and non-physical impairments’ is acknowledged as pivotal in identifying rehabilitation needs and organising rehabilitation referrals as necessary. The AHA scientific statement includes additional recommendations for the pre-discharge assessment, suggesting a ‘discharge checklist’ covering different domains, such as cardiovascular, neurological, social, affective and other domains.10
There is no mention in these guidelines of who should complete the follow-up (previous ERC guidelines had suggested a physician or specialist nurse).36 It is suggested that this process should be systematic, indicating that all survivors – including those with previously identified rehabilitation needs – should be invited for follow-up assessment.9
Rehabilitation strategies and outcomes for survivors of OHCA with a severe hypoxic-brain injury have been previously described, and the needs of this highly complex cohort extends beyond the scope of this document.37 Follow-up services for OHCA survivors that comply with at least some aspects of the ERC guidelines (including systematic assessment and a focus on cognitive and emotional problems) have also been described.38,39 More services may exist, but there is currently no comprehensive reporting of this, particularly across the UK. A Swedish survey reported major variations in follow-up practices, with most centres offering a cardiology review only and no structured offer of support for cognitive and psychological issues.40 National guidelines were published in Sweden to try to standardise follow-up care, but to date no other country has done the same.41
In the absence of structured and standardised post-discharge support, it is not surprising that evidence supporting the effectiveness of rehabilitation programmes after OHCA is limited. The largest randomised controlled trial to date, conducted by Moulaert et al., indicated that an early post-discharge (within 1 month), 1 hour, nurse-led intervention focusing on cognitive and emotional assessment, provision of information and promotion of self-management strategies led to improved quality of life measures at 1 year post-cardiac arrest.24,42 Referral to specialised care and further follow-up sessions were offered if necessary; however, the requirement for this was infrequent.24,42 The Essex Cardiothoracic Centre has also described a follow-up intervention focused on the systematic assessment of psychological, cognitive and medical problems of OHCA-survivors and their carers in the first 6 months post-arrest; although overall health improved at follow-up, the lack of a control group does not allow evaluation of the effect of the intervention.39
What Do Patients Want?
Surveys of patients’ and families’ subjective experience of follow-up programmes and their own expectations around follow-up care are lacking. In a large qualitative survey, most survivors reported that no information was provided around what to expect after discharge, that the follow-up appointment was centred on cardiovascular issues, and that mental health issues were the least addressed with no mental health support being provided.43 They also indicated they felt differently from those who had experienced MI and would have appreciated connecting with “someone who had also gone through it.”43 In a recent pilot study, survivors also reported a mismatch between the actual and expected follow-up experience, with over 40% reporting that they would have liked to see another professional in addition to cardiologists and nurses (such as psychologists, occupational therapists and physiotherapists) and identifying issues of mental health, fatigue and cognition as high priorities to address at follow-up.30
A qualitative survey of relatives of OHCA survivors identified dissatisfaction and frustration concerning a lack of information about what might be expected after discharge and lack of follow-up and poor continuity in healthcare, as well as feelings that their own experience had been neglected.44 This study identified a need for bespoke booklets describing the cardiac arrest, intensive care unit stay and the importance of continuing care directed both to patients and co-survivors, with a multi-disciplinary approach focused on both cardiac and neurological recovery.44 Recent research has also identified that family members have specific information needs around how to support the survivor after discharge, as well as on how to cope with the transition from hospital to home.45,46
British Cardiovascular Intervention Society Proposal for Minimum Standards of a Structured Follow-Up Programme after OHCA
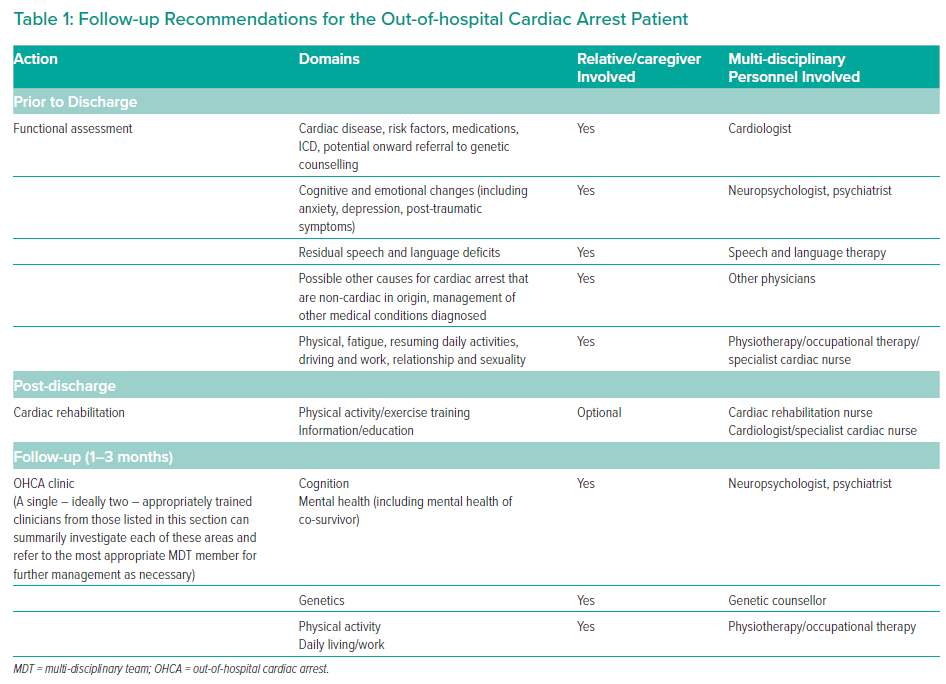
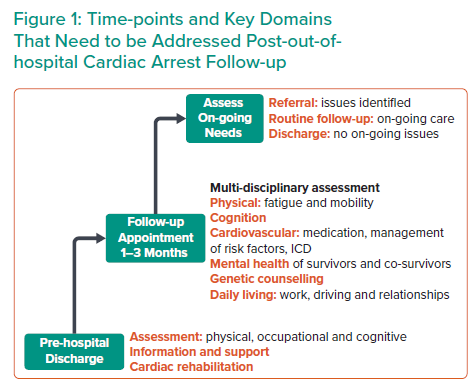
Based on current evidence and on the latest set of recommendations, we suggest the following approach (essential and desirable actions) for a systematic follow-up of All OHCA patients, regardless of cardiac arrest aetiology, and regardless of conscious state at time of hospital admission (Figure 1, Table 1). It is acknowledged that the majority of OHCAs are due to a primary cardiac aetiology but that there are several other causes of OHCA that should also be offered similar rehabilitation services. While it is accepted that some OHCA survivors may not share risk factors or lifestyle issues with their peers (e.g. younger survivors, those with good functional recovery), they may still benefit from cardiac rehabilitation to access psychological support and lifestyle advice more tailored to their individual needs and peer-to-peer networks. Future goals should be focused on providing specific OHCA survivor rehabilitation clinics with focus on specific requirements that are outside of the scope of this document but may require specialist input.
Before Discharge
Essential
All patients who have suffered OHCA should be offered a physical, cognitive and mood assessment prior to discharge. We recommend the creation of a dedicated MDT; this should include – as a minimum – occupational therapy, physiotherapy, cardiac rehabilitation nursing and neuropsychology. Each of these disciplines should assess OHCA survivors as appropriate. Streamlined access to other professionals is highly encouraged: these include speech and language therapists for cognitive-communication problems, cardiologists for cardiac therapy/referral to genetic counselling and other specialty doctors as needed. The assessment completed prior to discharge should be proportionate to survivors’ ability to engage and to their expected level of functioning after discharge (based on pre-cardiac arrest level of functioning). When choosing assessment tools for cognition, clinicians should be aware that memory, attention and executive functions are frequently impaired. Rehabilitation expertise should be sought where deficiencies are identified and a clear system for making referrals is recommended, as cardiac, neurological and psychological domains may all need attention.
Information leaflets designed specifically on cardiac arrest explaining expected difficulties in the early phases (pre- and post-discharge) for both survivors and co-survivors should be provided. These should include basic information relating to underlying cardiac conditions, medication, fatigue, memory/thinking problems, anxiety, low mood, living with and ICD and some recommendation around return to work/previous daily activities (including driving). Patients and their relatives should also be made aware of national support groups and of any local initiative to bring together survivors of OHCA. Consideration should be given to the fact that some patients and relatives may prefer accessing this information on a dedicated website or watching it in video format and, where available, they should be directed to this. A valuable source of peer-to-peer support and dedicated information provision including leaflets, videos and blogs is www.suddencardiacarrestuk.org. More detailed information is usually inappropriate at this stage as patients may still be experiencing memory problems, and relatives might still be in a state of shock following the event, therefore potentially limiting understanding and retention.10
Desirable
It is recognised that some survivors and relatives may have further questions on issues caused by the cardiac arrest after hospital discharge but prior to the follow-up appointment. It would be desirable that a member of the follow-up MDT could be contacted via a dedicated email or direct-dial telephone number to offer advice and guidance.
After Discharge
Cardiac Rehabilitation
All cardiac arrest survivors should be offered access to cardiac rehabilitation programmes – either group or home-based – regardless of the aetiology of their cardiac arrest. Although many survivors reported experiencing different issues compared to other MI patients, the core components of cardiovascular disease prevention and rehabilitation programmes remain central to maintaining good clinical outcomes of this group.47 The ambition should be that OHCA-specific rehabilitation programmes will be developed in the future.
Follow-up Appointment
Essential
It is acknowledged that there will be different modes of delivery of this service. We recommend that at least one, but possibly two, appropriately trained members of the MDT described earlier should be present at follow-up and complete a multimodal assessment of physical and non-physical elements as detailed below in the Content of the Follow-up Appointment section. A system to provide timely access to other professionals within the MDT is paramount to investigate any identified issue; this could involve on-call access, regular MDT discussions or another appropriate referral system. This would allow timely referrals to external services if required.
Follow-up appointments should be offered within 1–3 months after hospital discharge. In most cases these will be completed in the hospital where the patient was treated following the cardiac arrest; however, they could be carried out in a community setting where appropriate, or virtually via secure consultation platforms. We recommend that both the survivor and co-survivor where appropriate are invited to the appointment and we recommend allocating around 45–60 minutes for each appointment.
Content of the Follow-Up Appointment
The follow-up appointment should include the provision of information and support for survivor and family member, screening for emotional problems and fatigue, screening for cognitive problems and evaluation of any outstanding cardiovascular issues, including consideration of referral of genetic testing and the impact on the patient’s daily living.9 A checklist should be used to make sure all the following main domains are covered during the follow-up (Table 2).
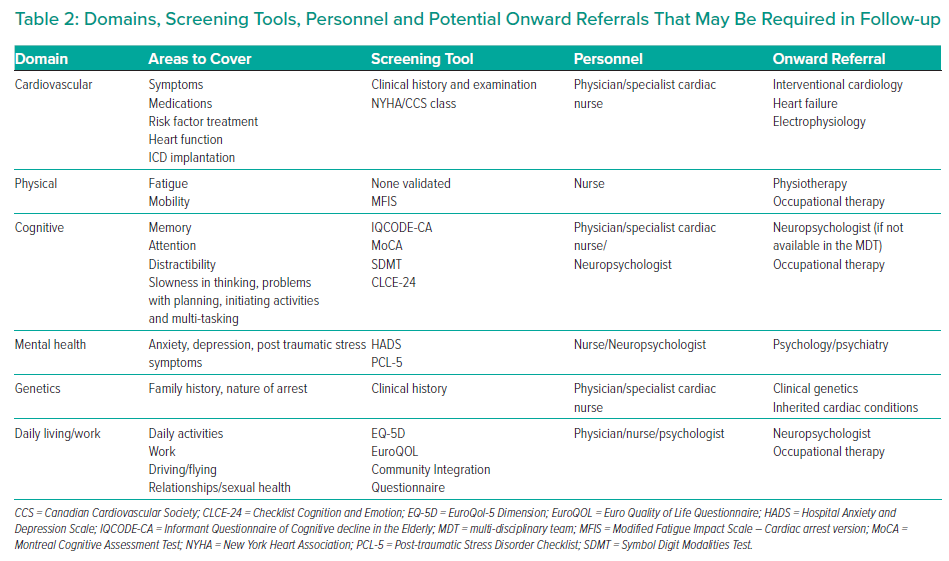
Physical
An assessment of fatigue and mobility should be performed. There is currently no validated tool for screening fatigue. We recommend investigating this at least qualitatively during the follow-up and consider a referral to occupational therapy if this is reported as a disabling symptom impacting on day-to-day life.
Cognition
We recommend asking the survivor about common complaints such as memory problems, attention difficulties, distractibility, slowness in thinking, word-finding difficulties, problems with planning, initiating activities and multi-tasking.8 Formal screening using a validated tool (such as the Montreal Cognitive Assessment or the Symbol Digit Modalities Test) is recommended. However a normal performance on this test should not prevent a referral to a neuropsychologist if the survivor reports on-going cognitive problems interfering with day-to-day activities. Collateral information should be collected as appropriate with the help of a family member/relative.
Mental and Emotional Health
We recommend exploring symptoms of anxiety, depression and post-traumatic stress in both the survivor and the family member/relative attending the appointment. The use of validated questionnaires should be considered. The Hospital Anxiety and Depression Scale and PCL-5 (post-traumatic stress disorder checklist for DSM-5) have been found useful, but other validated tools may be appropriate. If significant problems are identified, a referral to local mental-health services should be considered.
Cardiovascular
Eighty per cent of OHCA patients have a primary cardiac aetiology and so similar considerations to the non-arrested patient in areas such as coronary artery disease, structural heart disease and electrophysiology. For these patients, areas that should be addressed include risk-factor treatment, care post-percutaneous coronary intervention and medication review. Several patients will have non-acute coronary syndrome related admissions and may require onward referral to specialist heart failure services or may have an ICD and require on-going electrophysiology care.
Genetics
Survivors of OHCA may have significant underlying inherited cardiac conditions such as cardiomyopathy or channelopathy. In cases where the cause of the cardiac arrest is unknown, onward referral to a clinical genetics/inherited cardiac conditions clinic should be considered.35
Daily-living and Work
A full assessment of return to daily activities, driving, work and impact on relationships and sexuality is recommended. Accordingly, support with information leaflets can be provided.
Additional Follow-ups
It is acknowledged that many survivors and relatives will not need further follow-up, provided that all relevant areas have been covered and appropriate referrals made.
However, it is also acknowledged that some survivors and co-survivors may encounter OHCA-related difficulties at a later point – for instance, when returning to work, to driving or normal day-to-day activities. We recommend that survivors are given the option to self-refer back to the follow-up clinic or to be referred by their general practitioner. These referrals should be screened by the MDT and accepted, rejected or redirected to other services as appropriate.
In addition, a small number of survivors and their families may benefit from an additional appointment after their first visit, which should be offered at an appropriate point in time within the first year. This may include a need for specialist medication review or monitoring of cardiac arrest related problems that did not trigger a referral to specialist service(s) in the first review but were noted to cause significant strain.
Documentation and Auditing
After follow-up, a clinic letter should be sent to the survivors’ general practitioner, the survivors themselves, and other relevant parties as appropriate. Auditing of the follow-up clinic is strongly encouraged. Survivors and co-survivors should be provided with a brief patient reported outcome measure (PROM) to evaluate their satisfaction with the service. This could be offered at the point of discharge from the clinic, either at the end of the appointment or after receiving a copy of the discharge report. Different formats should be used as appropriate (paper, electronic). The PROM should also seek patients’ opinions around options for service improvement. The group recognises that there is limited evidence in this area and that as rehabilitation services are established, a parallel research stream should be developed across the UK to collaboratively address these gaps with a view to further informing National policy.
Summary and Vision
This document presents an up-to-date set of recommendations for best follow-up practice following out of hospital cardiac arrest, based on current available evidence. These recommendations incorporate and expand on current ERC guidelines, suggesting the creation of follow-up MDTs where different professions (cardiology, nursing, occupational therapy, physiotherapy and clinical psychology/psychiatry) collaborate in the assessment of survivors’ and relatives’ needs, and have awareness of the specific support networks and referral pathways accessible for this vulnerable cohort of patients.
Specific guidance is provided regarding pre-discharge assessments and provision of information, and a strong focus is placed on the importance of auditing the service, regularly collecting PROMs, and linking up with other follow-up clinics locally and at a national level along with peer-to-peer support networks to improve outcomes after cardiac arrest survival.