The Challenge
Only 2% of ischaemic stroke patients in the UK receive emergency interventional thrombectomy treatment.1 More than 7,000 eligible patients each year are unable to access a therapy that might prevent life-changing disability.
The Aim
To contribute to a national solution, allowing equitable access for all eligible patients to stroke thrombectomy treatment. The aim of our document is to describe the potential contribution that UK interventional cardiologists (ICs) could make to the current unmet need of providing a 24/7 mechanical thrombectomy (MT) service for all suitable stroke patients. This initiative is motivated by:
- An awareness of the clinical effectiveness of MT.
- The difficulty in providing MT to as many patients as possible using existing trained specialist groups.
The Case for Interventional Cardiologists Performing Mechanical Thrombectomy in the UK
Between April 2019 and March 2020, Sentinel Stroke National Audit Programme (SSNAP) data reported 89,280 strokes in the UK, of which 77,735 were due to cerebral infarction. An estimated 10−12% of these strokes would in theory be candidates for emergency MT. Despite a well-established infrastructure of specialist stroke care centres, only 1.57% of these patients received this potentially life-changing treatment.1
Until 2014, reperfusion treatment for ischaemic stroke was primarily through IV thrombolysis, even though this is a relatively ineffective treatment for large vessel arterial occlusion. In terminal internal carotid artery thrombotic occlusions, successful recanalisation with thrombolysis occurs in as few as one in 10 cases.2 Better methods of reperfusion are therefore clearly desirable.
In 2015, multiple randomised controlled trials began to show large benefits from reperfusion of cerebral circulation through the strategy of systemic thrombolysis followed by immediate MT. A meta-analysis of these trials showed a number needed to treat (NNT) of 2.6 to achieve a one-point improvement in the modified Rankin score (where 0 is no disability and 6 is dead).3
Treatment has further evolved over the last 6 years and a comprehensive review of the evidence was undertaken by the National Institute for Health and Care Excellence in 2019.4
Current recommendations are:
- To offer thrombolysis and thrombectomy for anterior circulation strokes presenting before 6 hours.
- Following the publication of the results of DAWN and DEFUSE III, to offer thrombectomy for those presenting up to 24 hours with salvageable brain tissue on diffusion-weighted MRI or CT perfusion scanning.5,6
The UK does not provide this care pathway to most suitable patients and remains far behind the best services in Europe in MT provision. While other aspects of MT infrastructure do require attention – and are receiving this via the Integrated Stroke Delivery Networks (ISDNs) – the problem in the UK is manifestly that there are too few trained operators.
Current Infrastructure Challenges
Imaging and Reporting
Patients who are face, arm, speech test (FAST) positive are currently recognised pre-admission and conveyed to the nearest hospital by ambulance, along with many ‘stroke mimics’ – patients who present with symptoms initially thought to be secondary to acute cerebral ischaemia but are subsequently found to have an alternative, non-vascular aetiology. Most undergo urgent CT scanning and are assessed by the emergency department (ED) or stroke team as an emergency so that a default strategy of thrombolysis can be considered.
Patients should also be considered as potential candidates for MT based on their clinical presentation and CT angiography results. Unfortunately, while CT angiography could technically be undertaken in all hospitals, radiological expertise for reporting the results is not currently available on a 24/7 basis across the UK.
However, if scans can be undertaken, the diagnostic skill set can be relatively easily acquired locally or alternatively be delivered through remote expert support, with or without the assistance of artificial intelligence (AI) software.
A national optimal stroke imaging pathway has been developed based on best evidence, investment in both training and AI has been secured at a national level, and a digital lead appointed to ensure that all regions gain equitable access to appropriate imaging.7
Specialist Intervention Facilities and Sharing Resources
Only three hospitals in the UK provide 24/7 stroke thrombectomy services, while only four offer MT at the weekend. By contrast, in 62 hospitals, cardiac catheter lab facilities are available for heart attack interventions, 24/7 365 days a year, with dedicated teams of nurses, radiographers, physiologists and consultants delivering reperfusion in 27,000 primary percutaneous interventions (PPCI) for ST-elevation MI (STEMI) per year, the default strategy for occluded coronary vessels since 2009.
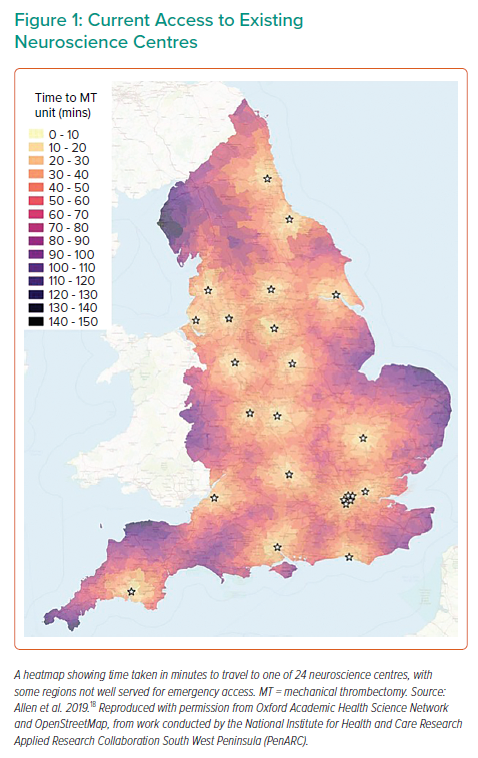
Current planning regarding the optimal location of stroke thrombectomy centres is that MT should be provided 24/7 at all 24 established neuroscience centres in England with existing interventional radiology services, expertise and a co-located hyperacute stroke service.8,9
Even if this can be achieved, this will leave some regions without timely cover for treatment, thus requiring between four and seven other non-neuroscience MT centres for full geographical coverage (Figure 1). This process mimics the evolution of PPCI for STEMI, which started in pioneering centres and then spread across the country until all geographical areas were adequately covered. In the meantime, stroke coverage will likely be achieved in some regions by use of the well described ‘drip and ship’ approach.10
The challenge to this approach is familiar to those who witnessed the development of PPCI and the delays involved in a patient being transferred from one ED to another for a time-sensitive intervention. Specifically, the median door-in to door-out time at referring stroke centres is currently 2 hours and 10 minutes, with a further 40 minutes transfer time.1
With the NNT in MT being so much more favourable than for PPCI, and the even more time-sensitive nature of cerebral infarction compared with MI, establishing equitable access to MT facilities for patients across the UK is a priority and one which may only be achieved with radical new approaches involving the sharing of interventional facilities and operator skills.
Workforce Challenges
The composition of the workforce delivering MT varies across the world, with cases delivered by interventional neuroradiologists, interventional vascular radiologists, neurologists, neurosurgeons and cardiologists. By contrast, thrombectomy in the UK has thus far been delivered almost exclusively by interventional neuroradiologists (INRs). While highly expert, their numbers are too few to plausibly deliver 24/7 MT services across the UK.
At the time of writing, 81 INRs are currently providing MT with 7 INRs scheduled to complete training in 2020 with a further eight completing in 2021. The Royal College of Radiologists has estimated that at least 50 more INRs would need to be trained in the UK to deliver an equitable service, giving 120 in total. Given the paucity of 24/7 rotas in existence for MT, it seems unlikely that round-the-clock coverage will be achieved by simpy adding 50 more INRs. By contrast, to provide a PPCI service to all patients across the UK, 713 consultant ICs are registered in the UK, with the significant majority of those participating in a 24/7 rota at an average intensity of one in seven. The British Cardiovascular Interventional Society (BCIS) Sustainable Workforce document recognises that to maintain a 24/7 rota with a maximum on-call frequency of 1:6 and a half-day compensatory rest after a night on call, a minimum of six (and ideally eight) operators are needed.
In addition to the generic challenges of medical workforce expansion, if the UK relied solely on the expansion of the INR team to deliver treatment for stroke, there are a finite number of aneurysms, arteriovenous malformations and fistulae to be addressed. One potential consequence of this could be that the procedural volumes per operator for these other important activities would fall, which may not be desirable.
Looking at the workforce calculations from a centre perspective, if MT was to be provided in the 24 neuroscience centres and all thrombectomy operators agree to contribute to an out-of-hours on-call, then between 144 and 192 operators would be needed. For 8,000 cases, this would equate to 40–55 MT cases per operator. Expanding to 30 centres (according to the geographical considerations above), the numbers would be 180 to 240 operators each doing 33–44 thrombectomy cases per year.
It becomes obvious that new approaches are going to be needed as there will be insufficient INRs to deliver the service to provide an equitable MT service throughout the UK within the next few years. However, the aspiration to achieve a nationwide 24/7 MT service within the next 2–3 years could be realised if 120 existing willing ICs were trained to contribute to the service.
Meanwhile, every 2-year delay in implementing a nationwide service is likely to contribute to more than 10,000 UK stroke patients experiencing avoidable long-term disability. Given that the first major randomised trial to show the life-changing benefits of MT was published on 1 January 2015, further delay should no longer be considered reasonable, in our view, when other mechanisms of delivery have been shown to be safe and successful in other countries.11
Interdisciplinary Solutions
Solutions to this problem have already been conceived and delivered in other countries in Europe and further afield. In St Petersburg, an interventional stroke programme was set up in 2015 using the existing STEMI network, cath labs and ICs.11 This was delivered through a programme of training sessions and masterclasses delivered by neurointerventionalists to the region’s ICs. Prior to this initiative, only 25 patients per year were being treated with MT. Now, by using the combined skills of INRs and ICs, the programme treats 650 cases per year with MT, reporting successful reperfusion in 81% of cases.11
Models and network solutions are likely to vary across different UK regions. For example, in London dedicated interventional neuroradiology centres could provide 24/7 MT by pooling the existing INR teams. In other regions, however, it may be that hybrid services are offered within neuroscience centres by a combination of existing INR teams with operators from other specialties. Finally, in non-neuroscience centres with geographical barriers to services, using existing coronary/vascular interventional facilities and operators makes more sense, given that many are already providing 24/7 emergency cover and are well placed to provide timely stroke thrombectomy to their own populations.
If non-neuroscience centres were to develop, it would require a hub-and-spoke network model, with the local hybrid MT team working and training closely with their neuroscience centre colleagues and running a joint programme. This joint working, designed flexibly according to the needs of each region, will help bridge the current gap in available operators.
Three hospitals in the UK have successfully implemented an MT service with the joint efforts of INRs, ICs and/or radiologists, the most recent of these being Dundee, where the first patient was treated in November 2020. Thus far, the inability to achieve this elsewhere in the UK is due to lack of capacity in the national training programme and lack of agreement as to exactly how to train non-INRs in MT.
The principal proposal by this BCIS Stroke Thrombectomy Focus Group is a two-part bespoke training programme to be made available to interested ICs to expand the available pool of active MT operators:
- Stage 1: training of established consultant ICs.
- Stage 2: training in a structured programme, at home or abroad, for IC trainees after they achieve the certificate of completion of training.
While expanding the trained workforce, BCIS will help to encourage and support the development of solutions for access to patients across the UK, as was undertaken for PPCI.
Why Interventional Cardiologists?
Despite their lack of experience in the cerebrovascular system, ICs have an extensive interventional skill set for the delivery of percutaneous, catheter-based techniques for coronary and valvular procedures. ICs are therefore well placed to be trained in the anatomical and technical challenges associated with MT. Similarly, vascular radiologists are well placed to learn these skills, though there are fewer of them than ICs.
It has also been proposed that training could be offered to non-catheter specialists with an interest in stroke, such as neurologists or stroke physicians. There is certainly no theoretical barrier to this, though without a baseline interventional skill set, the training programme would inevitably be much longer than for ICs. Additionally, IC are already highly experienced in emergency, time-sensitive pathways, and the management of critically ill, conscious patients during interventional procedures.
In some areas, such as radial artery access, the use of adjunctive antiplatelet medication, and the ongoing investigation of the cardiovascular system to look for the causes of stroke, IC experience could also enrich the current MT pathway.
As with INRs, ICs have demonstrated their ability to adapt and excel at the delivery of new procedures as they have evolved. New coronary techniques and valve interventions have advanced rapidly within the timeframe of all practising consultant’s careers. These include the shift of more than 90% of UK PCI procedures from femoral arterial access to radial arterial access and the improvement of chronic total occlusion (CTO) techniques, such that CTO success rates have risen from 50% 10 years ago to over 90% in specialist centres.
ICs have also successfully delivered entirely new fields, such as transcatheter aortic valve implantation, MitraClip, patent foramen ovale closure or percutaneous atrial septal defect closure. Some ICs also have experience in carotid stenting, which is considered advantageous for accelerated training by European training bodies.12 The development of these fields has largely been through workshops and then expert proctoring. Consultants were not asked to take long periods of absence from their existing roles and yet delivered high-quality, safe new services.
Crucially, most ICs are also already part of a 24/7 rota and most are content to make this part of their working pattern throughout their consultant career. A recent survey sent to the membership of BCIS revealed that 192 respondents (52%) would be very keen to contribute to a stroke thrombectomy service as part of a 24/7 rota if appropriate training were available, with further respondents also willing to consider it.13
Perhaps the strongest argument for a national interdisciplinary solution is the existing, established, UK-wide emergency interventional cardiology network. It seems unlikely that the country can afford to have another 24/7 team of clinicians, nurses, radiographers and a lab on standby 24/7 in more remote locations, when this already exists to cover the UK for STEMI.
Agreement in Training Interventional Cardiologists
There is an important discussion to be had about the ideal training approach and duration of MT training for an IC consultant. Given the successful programmes elsewhere in the world, we can be confident that the previously proposed estimate of 2–3 years’ training time are unduly pessimistic, but factors that will need to be taken into account during this national discussion will include:
- Who can dictate how many ICs can or should be trained?
- How and by whom would competence be certified?
- How to fit practical training into an IC consultant’s job plan.
- Can this be replaced by dual accreditation for trainees in the future?
Many of the relevant discussions regarding training are ongoing in other countries.12 Agreement of specialist bodies will be required for medicolegal reasons, and safe and speedy delivery is strongly in the interest of the population. The political challenge regarding the barriers to delivery will require skill and diplomacy from those who oversee the provision of healthcare, given the different perspectives in this area.
Methods of Training Interventional Cardiologists
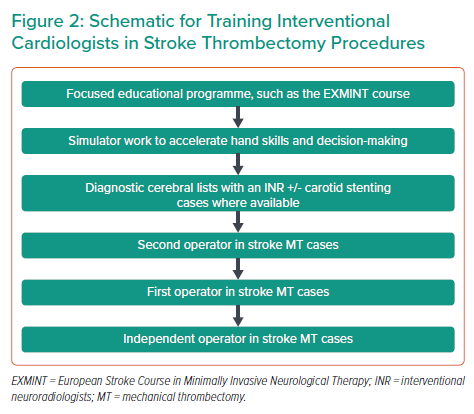
Given the starting point of low case numbers, the need to train INRs in the UK to be ready to carry out and run MT programmes, and the current job plans and curriculums in cardiology, it is clear that a bespoke programme will be required to train ICs, depending on whether they are based in existing neuroscience centres. A schematic of how such a programme might look is shown in Figure 2.
Training a physician with minimal cerebrovascular experience to perform MT on a real patient on day 1 is no longer how contemporary training works. Focused theoretical training followed by simulator work (which has advanced enormously over the past decade) is the standard mechanism of training new operators in interventional procedures in the modern era. Operators could then further develop their skills through diagnostic cerebral work or carotid stenting, where available, before becoming a second operator on MT cases, and then a first operator on stroke MT cases. Pathways such as this have been shown to be successful both inside and outside the UK.
Theoretical courses already exist in this area. For example, the European Stroke Course in Minimally Invasive Neurological Therapy (EXMINT) programme is run by the European Society of Minimally Invasive Neurological Therapy and is endorsed by the European Stroke Association.14 This is a 2-week programme, exam and viva assessment covering the anatomy, pathophysiology and imaging components of relevance to highly specialised procedures in the brain. It is specifically designed for the training of non-INRs in MT by experts in the field and the procedure.
Simulator training has advanced rapidly in all interventional fields, and MT simulation suites are now available in two locations in the UK, offering a variety of cases from simple to difficult anatomies and allowing training on each procedural step. The operator can select a range of cath lab equipment, including catheters, balloon/aspiration catheters, wires, stents and stent retrievers. The ANGIO Mentor suite (Simbionix) is a human size simulator allowing multidisciplinary stroke team training, and the PROcedure Rehearsal Studio (Simbionix) software enables the creation of an unlimited library of cases based on real patient DICOM data. Neurointerventional simulation training has already been shown to be effective in high-risk endovascular procedures and in-built automated scoring systems within the simulators have even been demonstrated to be able to discriminate between levels of operator proficiency for carotid artery stenting.15–17
Case numbers and credentialling are perhaps the most challenging area in which to achieve consensus before ICs could contribute to an interventional stroke service. In most areas of specialist medical training, evidence has steered us away from a numbers-based assessment to a competency-based one. With such time-sensitive procedures, however, there is no doubt that experience of a variety of scenarios and management of complications will lead to improved performance. A minimum number of simulated cases and real-life second operator MT cases seems appropriate, but personalised, mentored training with assessment of competence by one or more experienced operators is in keeping with contemporary medical and surgical training.
Maintaining skills and case numbers is essential but will likely become less of an issue (as will numbers to train on) as the indications for this therapy continue to expand. In addition, while volumes of stroke thrombectomy cases are vital to maintaining skills, once a focused early period of training is completed, ICs are high volume catheter specialists already, accessing head and neck vessels when catheterising left and right internal mammary artery grafts, as well as managing radial and femoral access sites, periprocedural anticoagulation, microcatheters, aspiration catheters, stent delivery, specialist wires, telescoping techniques and many other transferrable skills that will support maintenance of MT skills.
MT numbers undertaken by operators in comparable European countries would suggest that volumes of approximately 30 per operator per annum are adequate for maintaining skills, which fits well with the workforce calculations outlined above.
Conclusion
The efficacy of MT in patients with anterior circulation stroke caused by large vessel occlusion is long established. Given the life-changing effect of successful MT, equitable access to this therapy is now required. Over 6 years have passed since the first positive randomised controlled trial reported and the UK is still not offering this treatment to the more than four out of five patients who could benefit. This is principally because of a lack of trained operators, as all other barriers are readily surmountable.
ICs have transferrable skills in this area, which could significantly shorten the training time required for new catheter specialists to acquire the hand and cognitive skills to train in percutaneous therapies from scratch. Many ICs are willing to provide this vital service in the UK on a 24/7 365 days a year basis, through interdisciplinary, collaborative working. This would also provide additional infrastructure currently used to deliver one of the safest and most comprehensive interventional heart attack services in the world.
The BCIS endorses the aims of this document – to facilitate the training of ICs to contribute to the national stroke MT service, offering safe, effective and equitable access to this essential treatment for all of our patients in a timely fashion.