Coronary artery ectasia (CAE) is an abnormal coronary artery segment dilatation commonly associated with atherosclerosis. It manifests as an abnormal coronary artery dilatation, characterised by an unusual enlargement of a coronary artery segment exceeding one-third of the affected coronary artery. In some situations the diameter of the ectatic (dilated) segment can exceed 1.5-fold the diameter of a normal adjacent segment of the same artery.1,2 Coronary artery ectasia is divided into four categories: type 1, widespread ectasia affecting two or three vessels; type 2, widespread ectasia in one vessel with localised disease in another; type 3, widespread ectasia confined to a single vessel; and type 4, localised or segmental involvement.3
CAE prevalence varies, but the current estimations range between 3% and 8% in patients undergoing coronary angiography.1,4,5 Coronary angiography and intravascular ultrasound (or optical coherence tomography) are the common techniques for visualising ectasia extent and any concomitant coronary artery disease (CAD) and guiding vessel placement, respectively.
That being said, CAE is a non-benign disease, with various studies associating it with ischaemia and acute MI.6,7 Medical experts classify CAE as either a subcategory of atherosclerotic CAD or a distinct entity, and this is a matter of contemporary debate. Despite its co-occurrence with atherosclerotic CAD, some experts consider CAE a separate entity.1,6,7 This is due to the MI association with CAE, even in the absence of obstructive lesions in the affected coronary arteries.2 More importantly, the question of whether isolated CAE without obstruction requires medical treatment is an uncertainty that is widely debated in the medical community.2 In situations when treatment is preferred, there is no clear consensus on the optimal management approach.2 This highlights the clinical significance of thoughtful evaluation and management in CAE patients.
In a recent case series, apixaban, a type of non-vitamin K antagonist oral anticoagulant (NOAC), was administered as a novel approach for managing massive intracoronary thrombosis, particularly in patients with ectatic coronary arteries and a significant thrombus burden. The decision to use apixaban was motivated by its use in the AUGUSTUS study, combining it with dual antiplatelet therapy (DAPT) in one of the treatment arms. This approach led to the successful resolution of thrombi in both cases, as confirmed by control angiography at the end of the first month.8
Case 1
A 36-year-old male patient with unknown chronic medical history was admitted to hospital. The reported symptoms included chest pain radiating to the back and both elbows, dizziness, sweating, one episode of vomiting, and dyspnoea.
The laboratory results were as follows: kidney function tests normal, creatine kinase-MB 35.50 IU/L (normal range 5–25 IU/L), and troponin T 0.785 ng/ml (normal range 0–0.01 ng/ml). The lipid profile assessment indicated elevated total cholesterol at 9 mmol/L, LDL cholesterol at 7.66 mmol/L, triglycerides (TG) at 1.65 mmol/L and HDL cholesterol at 1.01 mmol/L.
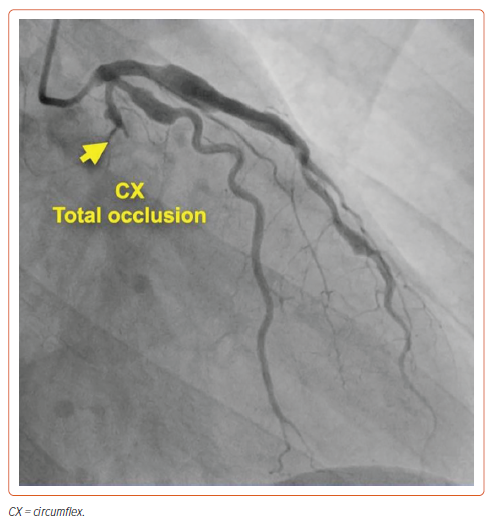
Normal ECG and echocardiogram were reported. During a cardiac catheterisation conducted upon admission, a proximal blockage in the left circumflex artery (LCx), along with ectasia in the obtuse marginal artery and the left anterior descending artery (LAD), were identified (Figure 1 and Supplementary Video 1). No stents were placed during the catheterisation.
Treatment
The patient was discharged and treated medically with a prescription of DAPT (aspirin 100 mg daily and clopidogrel 75 mg daily), apixaban 5 mg twice daily and atorvastatin 80 mg once daily.
Outcome
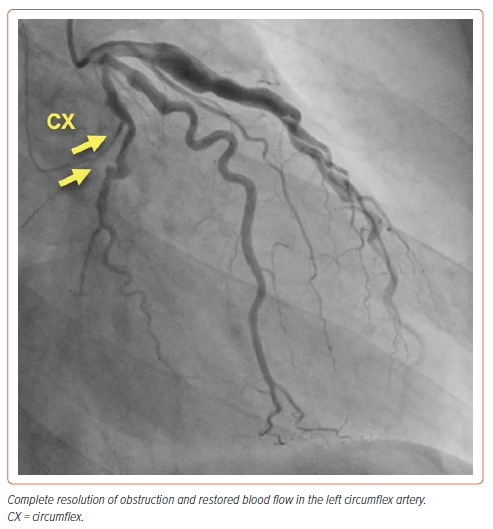
After 1 year, the patient was readmitted as a day case for an elective cardiac catheterisation to re-evaluate his coronary arteries (Figure 2 and Supplementary Video 2). The images obtained from this procedure indicated that the LCx artery occlusion had disappeared completely. The patient was then monitored through clinical follow-ups to track his progress.
Case 2
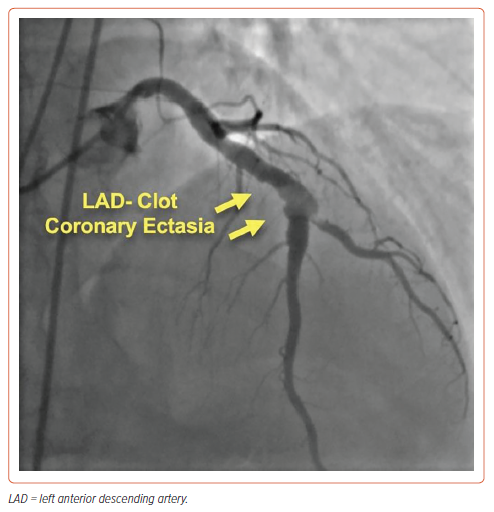
A 53-year-old man with a history of smoking but no other CAD risk factors presented with chest pains. The patient was diagnosed with non-ST-elevation MI. Echocardiography showed mild anterior wall hypokinesia with a 50% ejection fraction. On the following morning, coronary angiogram showed an ectatic LAD and a substantial thrombus at the major diagonal artery bifurcation, with preserved anterograde blood flow graded as thrombolysis in MI (TIMI) 3 (Figure 3 and Supplementary Video 3).
The patient was started on oral DAPT with aspirin 100 mg and clopidogrel 75 mg. In addition, IV tirofiban was administered for 48 hours to enhance thrombus dissolution.
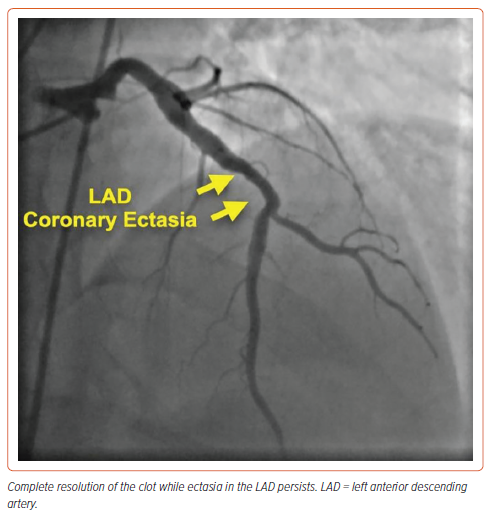
After the medical management, the patient reported remarkable chest pain relief. A repeat coronary angiogram conducted after 48 hours indicated no significant changes compared with the initial findings, signifying that the thrombus burden remained unchanged. He was discharged with the following medications: aspirin 100 mg once daily, clopidogrel 75 mg once daily, apixaban 5 mg twice daily, and atorvastatin 80 mg once daily. The patient was closely monitored, with clinic visits scheduled every fortnight. The patient’s clinical condition remained stable during the monitoring period, with no chest pain recurrence or other cardiovascular symptoms. Two months later, a coronary angiogram (Figure 4 and Supplementary Video 4) showed complete dissolution of the thrombus.
Discussion
CAE occurs when diffuse dilatation occurs in up to one-third of a coronary artery segment. The coronary artery is classified as having CAE when the diameter of the ectatic (dilated) segment measures more than 1.5-fold the diameter of a normal adjacent segment of the same artery.1,2 Atherosclerosis plays a significant role in the development of this condition. The tendency of CAE to co-occur with CAD suggests that CAE is potentially a unique form or subtype of atherosclerosis.7 Based on the current literature, CAE type 1 is associated with adverse events, such as myocardial ischaemia, even in the absence of obstructive lesions.3,6,9 The events manifest more when the ectasia affects a larger portion of the coronary arteries.6
CAE patients frequently have significant thrombus burden and initial flow reduction stemming from turbulent blood flow in dilated coronary segments.4,10 The turbulence leads to exercise-induced angina and MI, irrespective of the severity of concomitant stenotic coronary disease.4 In a substantial cohort of patients presenting with acute MI symptoms, the CAE rate is approximately 3.6%.10 This is a remarkable health challenge given that, on most occasions, CAE patients have angina symptoms and have an elevated risk of MI and sudden cardiac death.2
Management
Effective CAE management remains to be determined, especially in an isolated case. Despite being a subject of debate in the current medical literature, there needs to be more consensus regarding effective treatment or tailored guidelines for therapeutic intervention. Medical, percutaneous and surgical interventions are considered effective treatment options for the condition. However, there are no randomised controlled trials in the literature evaluating the efficacy of the various recommended therapies, complicating the decision-making process regarding CAE treatment choice.
Medical Therapy
The ideal medical therapy for CAE patients is the subject of ongoing debate. Addressing the cardiovascular risk factors associated with atherosclerosis is crucial for effective CAE patient management. Experts recommend managing CAE with NOACs. CAE patients have considerably elevated P-selectin, β-thromboglobulin and platelet factor 4, suggesting increased platelet activity levels compared with people with angiographically normal coronary arteries.11 This forms the basis for using antiplatelet therapy in CAE treatment. However, using either single antiplatelet therapy or DAPT is a widely debated medical subject.
The unique choice of anticoagulant for managing CAE remains uncertain, although warfarin has traditionally been prescribed for some patients.4 A study by Pranata et al. proposed that anticoagulant inclusion in CAE management can increase the effectiveness of the treatment compared with exclusive DAPT, particularly in cases of isolated CAE without other evident stenotic lesions.4
Then again, the addition of anticoagulation therapy is a broadly debated subject in CAE management. Other studies show that incorporating anticoagulation therapy can improve the management of the condition, especially when the patient has both CAE and acute coronary syndrome (ACS).12,13 NOACs are remarkably beneficial to CAE patients despite the absence of clinical evidence supporting their use. In this context, we report two cases in which a triple therapy approach (combining DAPT with NOACs) resulted in complete resolution of obstruction and clinical improvement of the CAE patients. The outcomes in the aforementioned two cases shed light on the effectiveness of these therapeutic interventions in managing CAE. More importantly, the findings are consistent with the current literature, which shows enhanced CAE management with the use of these therapies. Furthermore, despite the low generalisability of the findings, the case study evidence underscores the essence of clinical trials in establishing evidence-based guidelines for treating CAE, whether in isolation or in conjunction with coronary stenosis.
Percutaneous and Surgical Interventions
Percutaneous and surgical interventions are two common strategies for managing CAE. The former entails balloon angioplasty, adjunctive pharmacotherapy and placement of stents, while the latter incorporates coronary artery bypass grafting, coronary endarterectomy and aneurysm resection ligation. As indicated earlier, no robust evidence supports the use of any specific intervention in the context of CAE. The choice of therapeutic method depends on the patient’s anatomy, the extent of the ectasia, the severity of the symptoms and the overall health status. More importantly, the subjects of percutaneous and surgical interventions fall outside the scope of our current findings. Additionally, percutaneous coronary intervention in cases involving CAE and significant coronary stenosis and ACS presents unique challenges. It is associated with increased procedural failure and complications.12
Conclusion
DAPT, in combination with NOACs, has a high potential to enhance the management of CAE in selected patients.