Coronary computed tomography angiography (CCTA) is a noninvasive tool capable of directly visualising the coronary anatomy with high sensitivity and negative predictive value (NPV) for coronary artery disease (CAD) compared to invasive coronary angiography (ICA).1,2 Recent innovations in computed tomography (CT) technology have led to the rapid development of CCTA and its selection as an anatomic alternative to stress imaging.3 Despite this, CCTA alone cannot independently determine the haemodynamic significance of coronary stenosis, as compared with stress imaging, due to the low specificity for identifying coronary stenoses that induce ischaemia.4 This emphasises the unpredictable relationship between stenosis severity and ischaemia, which may provoke the need for unnecessary invasive coronary angiography (ICA) in patients who do not have ischaemia.5 For instance, patients undergoing CCTA with an intermediate lesion requiring ischaemia evaluation may have layers of additional testing, such as stress echocardiography, myocardial perfusion imaging by single-photon emission computed tomography, positron emission tomography or cardiac magnetic resonance image.6
Fractional flow reserve (FFR), defined as the ratio of maximum flow in a stenotic artery to maximum blood flow if the same artery were normal, is an invasive technique to determine lesion-specific ischaemia and can assist in guiding coronary revascularisation.7,8 Notably, in the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) trial, the use of FFR to guide coronary intervention compared with ICA guidance resulted in a 33 % reduction in major adverse cardiac events.9
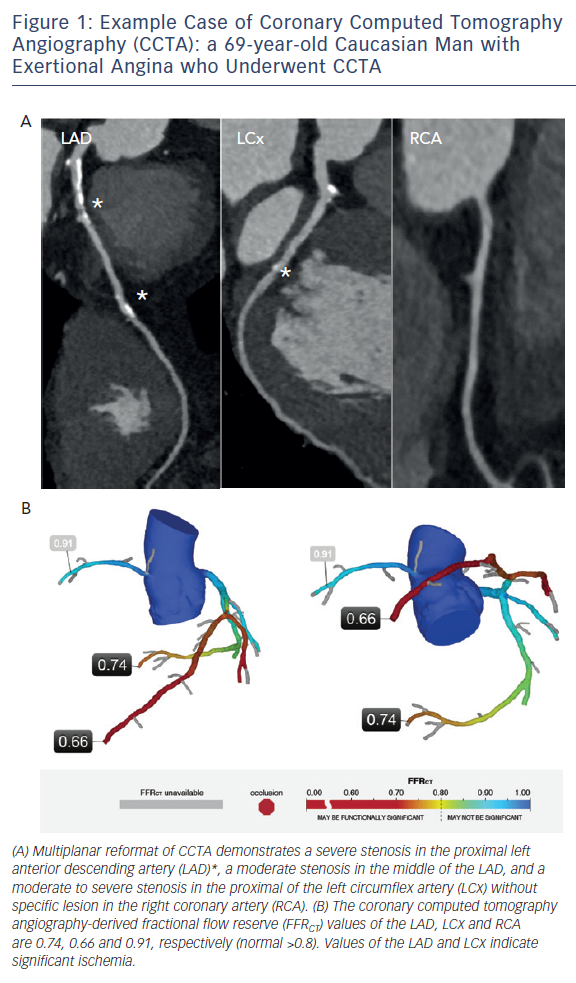
Recent advances in computational fluid dynamics enable the calculation of CCTA-derived FFR (FFRCT) from three-dimensional imaging anatomic models. Foremost, FFRCT reflects a novel imaging modality with the ability to determine the haemodynamic significance of CAD without additional radiation exposure or contrast injection beyond the initial CCTA (Figure 1). This review provides an overview of current evidence describing the appropriate use of FFRCT in the clinical setting, along with a discussion of the potential future directions of FFRCT.
Clinical Usefulness of FFR
FFR has been utilised to assess physiological function at the time of ICA in the cardiac catheterisation laboratory. The former procedure provides a reliable physiological index for determining whether coronary stenosis may cause ischaemia by measuring flow with a coronary guidewire before and after a visualised stenosis during maximal hyperaemia.10 A common definition of FFR is the maximal blood flow to the myocardium in the presence of a stenosis in the supplying coronary artery divided by the theoretical normal maximal flow in the same distribution.7 In current guidelines, a FFR value ≤0.80 is widely considered the threshold for revascularisation.
Numerous studies have confirmed the clinical benefit of utilising FFR in clinical practice.9,11–15 Revascularisation in the coronary arteries with a measured FFR of ≤0.80 was associated with improved prognosis, including a reduction in death rates, non-fatal myocardial infarction and urgent revascularisation when compared with ICA guided revascularisation alone or optimal medical therapy alone.16,17 Further still, Pijls et al. demonstrated in the DEFER trial that 5-year outcomes, and even 15-year outcomes, following deferral of percutaneous coronary intervention in the vessel of an intermediate coronary stenosis based on FFRs of ≥0.75 demonstrated excellent prognoses.11,18 In light of previous findings, current guidelines advocate a FFR-guided revascularisation strategy as a Class IA recommendation for identifying haemodynamically-relevant coronary lesions in stable patients, especially when non-invasive testing evidence of ischaemia is not available.19
Diagnostic and Clinical Performance of FFRCT
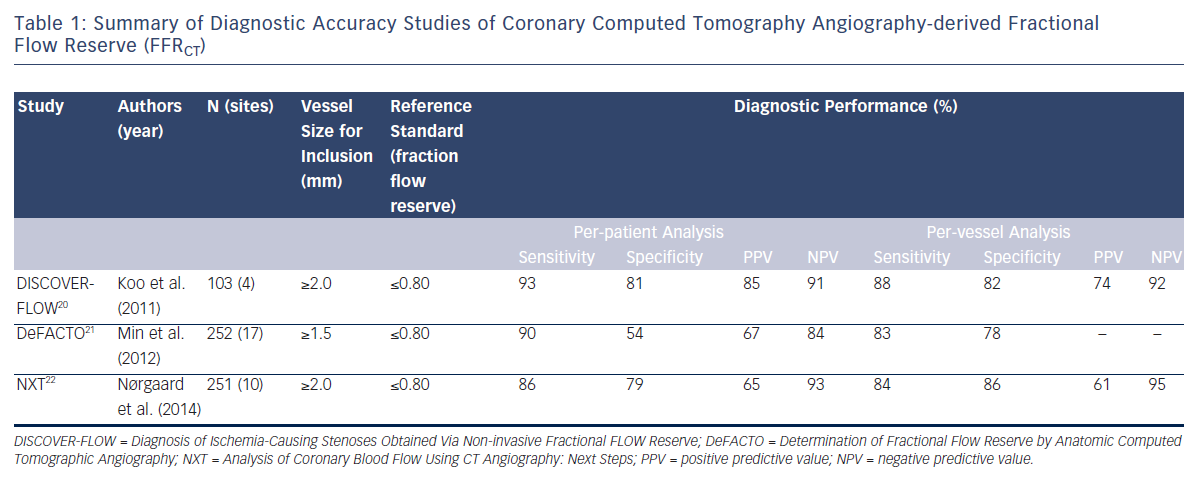
To date, three prospective multicentre trials, namely the Diagnosis of Ischemia-Causing Stenoses Obtained via Non-invasive Fractional Flow Reserve (DISCOVER-FLOW),20 Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography (DeFACTO)21 and analysis of Coronary Blood Flow Using CT Angiography: Next Steps (NXT)22 studies, have evaluated the diagnostic performance of FFRCT compared with invasive FFR as a reference standard. These studies are summarised in Table 1.
The DISCOVER-FLOW study was the first multicentre trial that assessed the diagnostic performance of FFRCT against ICA and invasive FFR. It included 103 patients with 159 measured coronary vessels from four sites in the United States, Europe and Asia.20 Anatomical obstruction was defined as a CCTA with stenosis ≥50 %, and either FFR ≤0.80 or FFRCT ≤0.80 was defined as ischaemia. In this study, both FFRCT and FFR correlated well on a per-vessel analysis according to Spearman’s rank correlation, reporting a coefficient of 0.72 (P<0.001). Further, utilising FFRCT on a per-vessel analysis revealed a diagnostic accuracy of 84.3 %, sensitivity of 87.9 %, specificity of 82.2 %, positive predictive value (PPV) of 73.9 %, and NPV of 92.2 %. The results did not differ materially on a per-patient analysis. Conversely, the accuracy, specificity and PPV were 58.5 %, 39.6 % and 46.5 %, respectively, based on a per-vessel analysis of CCTA; while a per-patient analysis demonstrated an accuracy of 61.2 %, specificity of 24.5 % and PPV of 58.0 %, respectively, according to CCTA. The area under the receiver operating characteristic curve (AUC) was 0.90 for FFRCT, which was superior to CCTA, which had an AUC of 0.75 (P=0.001), indicating a significant improvement in the discrimination of ischaemia.
The DeFACTO trial included 252 patients across 17 centres in five countries with the measurement of 407 coronary vessels. It was conducted to determine the accuracy of FFRCT in comparison with invasive FFR as a gold standard for the diagnosis of haemodynamicallysignificant coronary stenosis.21 On a per-patient analysis, FFRCT was superior in detecting ischaemia when compared with CCTA according to diagnostic accuracy (73 % versus 64 %), sensitivity (90 % versus 84 %), specificity (54 % versus 42 %), PPV (67 % versus 61 %) and NPV (84 % versus 72 %), respectively. In a patient-based analysis restricted to those presenting with intermediate stenosis (i.e. 30–70 % stenosis), sensitivity was significantly higher for FFRCT than for CCTA (82 % versus 37 %), without a change in specificity. In addition, FFRCT displayed superior discrimination for ischaemia based on a per-patient as well as per-vessel analysis when compared with CCTA, with improved AUCs (0.81 versus 0.68 and 0.81 versus 0.75, respectively; P<0.001 for all). Though DeFACTO was unable to meet its pre-specified primary outcome, which was a per-patient diagnostic accuracy lower bound 95 % confidence interval no worse than 70 %, the utilisation of non-invasive FFRCT plus CT among stable patients demonstrated improved diagnostic accuracy as well as discrimination in comparison with CT alone for the diagnosis of haemodynamically-significant CAD.23
Most recently, the prospective multicentre NXT trial evaluated the diagnostic performance of FFRCT in 254 patients, with 484 vessels being studied.22 On a per-patient analysis, diagnostic accuracy, specificity and PPV were markedly higher for FFRCT (81 %, 79 % and 65 %, respectively) versus CCTA (53 %, 34 % and 40 %, respectively) (P<0.001, for all). Similarly, on a per-vessel analysis the accuracy, specificity and PPV were 86 %, 86 % and 61 %, respectively, for FFRCT compared with CCTA (65 %, 60 % and 33 %, respectively) (P<0.001, for all), without disparity in sensitivity (84 % versus 83 %). In the same study, a subgroup analysis among patients with intermediate stenosis severity (i.e. 30–70 % stenosis) demonstrated that FFRCT was superior to CCTA on a per-patient level, with better accuracy (80 % versus 51 %), specificity (79 % versus 32 %) and PPV (63 % versus 37 %) (P<0.001, for all) observed. Moreover, the AUCs for FFRCT on a per-patient and per-vessel basis were 0.90 and 0.93 versus 0.81 and 0.79 for CCTA, respectively (P<0.001 for all), indicating superior discrimination for ischaemia on the background of FFRCT. In summary, findings from the NXT multicentre trial support the contention that adding FFRCT to CCTA might provide a more comprehensive anatomical and physiological assessment of CAD.
In previous studies, CT datasets were transferred so software applications could be run, and consequently hours of processing were required before the results were returned to the physician. To this end, recent studies have explored on-site prototype algorithms to compute FFR from CCTA, which in turn may enable a more efficient patient flow and reduce analysing time to within 1 hour.24–26 Among these studies, De Geer et al. demonstrated that the sensitivity, specificity, NPV, PPV and accuracy of FFRCT for detecting significant stenosis (FFR≤0.80) were 0.83, 0.76, 0.93, 0.56 and 0.78, respectively, on a perlesion basis, and displayed a Spearman rank correlation coefficient of ρ=0.77 (P<0.001).26 Although still in its infancy, these investigators have strongly emphasised that this software permits on-site assessment of FFRCT within clinically-practical time frames, and may therefore have the necessary potential to be performed in a clinical setting.
Recently, the Prospective Longitudinal Trial of FFRCT: Outcome and Resource Impacts (PLATFORM) trial compared a FFRCT-guided diagnostic strategy (n=297) with usual care (n=287) in 584 patients with new-onset chest pain and intermediate risk of CAD.27 Usual care was stratified by planned ICA or planned non-invasive testing prior to enrollment. In the planned ICA stratum (FFRCT-guided, n=193; usual care, n=187), ICA was cancelled in 61 % after receiving coronary CTA/ FFRCT results, because the rate of non-obstructive CAD by ICA was 12.4 % (n=24) in the coronary CTA/FFRCT arm versus 73.3 % (n=137) in the usual care arm (P<0.001), with similar cumulative radiation exposure and 90 days clinical event rates. This result was similar after applying propensity score matching for 148 patients in each group (e.g. 12 % for CTA/FFRCT versus 72 % for usual care, P<0.001). In the planned non-invasive testing stratum (FFRCT-guided, n=104; usual care, n=100), the rate of non-obstructive CAD by ICA was comparable in both arms (12.5 % versus 6.0 %, P=0.95). Overall, there was no significant difference in revascularisation in subjects allocated to CTA/FFRCT compared to usual care in either the planned non-invasive or planned invasive testing arms (P=0.29 and 0.58, respectively). The PLATFORM trial suggests that FFRCT may be a useful and safe gatekeeper to ICA, particularly for reducing the likelihood of normal ICA when used as an alternative diagnostic tool to guide care in patients with planned invasive catheterisation.
Principal Components for Determining FFRCT
The scientific principles for determining FFRCT have been described in detail elsewhere.28 In brief, FFRCT utilises a computational fluid dynamics approach to determine the FFR of three vessels from typically-obtained CCTA images without additional imaging, changes of image acquisition protocols, additional medication or radiation exposure.28 The computational fluid dynamics method enables the quantification of fluid pressure and velocity based upon laws of mass conservation and momentum balance, while also solving the equations of human blood flow when applied to CCTA.
Details regarding the steps involved in the calculation of FFRCT have been outlined previously,23 and are briefly described as follows: 1) the acquisition of CCTA and creation of patient-specific anatomical models; 2) the quantification of total and vessel-specific coronary flow; 3) the calculation of baseline microvascular resistance; 4) the computation of hyperaemic changes in coronary artery resistance; and 5) the application of computational fluid dynamics to calculate coronary flow, pressure and velocity during the stages of rest and hyperaemia. While it can take approximately 8 hours to calculate the results of FFRCT, the majority of FFRCT measurements can generally be calculated within a few hours, and it is anticipated that more advanced techniques in the field of FFRCT will eventually induce a substantial reduction in calculation time.
Further Study of FFRCT
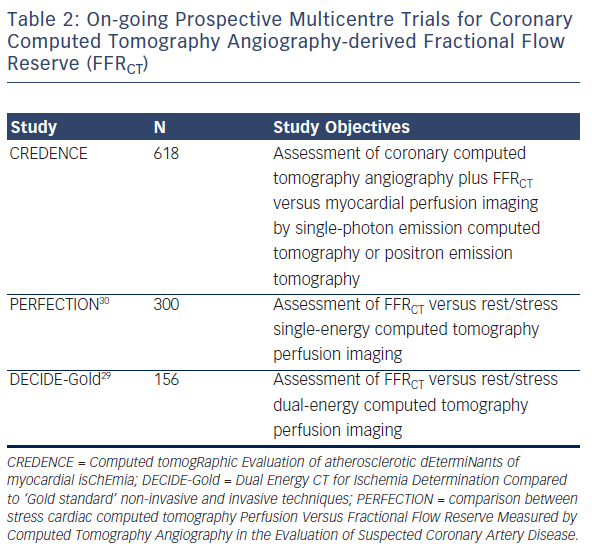
At present, studies related to FFRCT have mostly focused on its diagnostic performance for the determination of ischaemia, and comparisons of FFRCT with other stress imaging tests have not yet been implemented. To this end, several prospective multicentre clinical trials are currently on-going for the purpose of exploring the utility of FFRCT against other more established myocardial perfusion imaging procedures (Table 2). The upcoming Computed Tomographic Evaluation of Atherosclerotic Determinants of Myocardial Ischemia (CREDENCE) trial aims to evaluate the direct comparison of coronary CTA plus FFRCT with MPI by SPECT or PET (NCT02173275). Moreover, two other multicenter trials, the Dual Energy CT for Ischemia Determination Compared to “Gold Standard” Non-Invasive and Invasive Techniques (DECIDE-Gold)29 and the comparison between stress cardiac computed tomography PERfusion versus Fractional flow rEserve measured by Computed Tomography angiography In the evaluation of suspected cOroNary artery disease (PERFECTION),30 aim to assess the diagnostic power of FFRCT as compared with single/dual-energy CT perfusion stress imaging testing. The results of these trials will undoubtedly spark further interest in the clinical utility of FFRCT.
Current Limitations of FFRCT
Despite the recent approval of FFRCT by the US Food and Drug Administration for routine use in patients without known CAD in the clinical setting, there remain several considerations relative to FFRCT that should be emphasised. Foremost, impaired image quality is capable of affecting the susceptibility of FFRCT. This infers that significant motion, beam-hardening from calcified lesions and artefacts from irregular breathing can affect image quality. Moreover, irregular and/or high heart rate, as well as a high body mass index, can further impair the quality of CT images. Further, several important factors are required to determine the accuracy of FFRCT, including the mathematical models related to coronary flow, lumen size, vessel resistance and potential variation in the hyperaemic response.6 To date, the extant literature has mostly focused on data from patients with an intermediate risk of CAD in contrast to those with a high pretest probability for whom performing ICA is typically mandatory in light of the time-consuming process of FFRCT. To this end, although the computation of FFRCT often takes several hours, forthcoming innovative iterations improve this limitation.23 At present, whether the impact of FFRCT is influenced by symptom typicality remains to be elucidated, and underlines the importance of future studies to examine the connection between FFRCT and symptom typicality. Although previous studies have demonstrated positive results in terms of diagnostic performance, we may add that FFRCT might not reliably reproduce the data obtained when using invasive FFR. To this end, the most recent NXT trial using the latest version of computational fluid dynamics demonstrated a PPV of only 65 % based on per-patient analysis. As such, additional studies are warranted to reliably determine the clinical performance of FFRCT for detecting significant lesion ischaemia. In addition, the performance of FFRCT is not yet indicated in patients with a prior history of coronary artery bypass surgery or percutaneous coronary intervention with suspected in-stent restenosis. Forthcoming studies will advance our understanding through utilising further FFRCT development, including automated segmentation methods, machinelearning techniques and the refinement of the boundary conditions that underlie the FFRCT technology, thereby hopefully addressing the limitations of this method.23
Future Directions for FFRCT
Several potential studies should be considered in future research that utilises FFRCT. Beyond improved diagnostic accuracy, FFRCT may enable improved guidance for clinical decision making. Importantly, further studies will assist in determining the role of FFRCT as a gatekeeper to cardiac catheterisation as well as its impact on cost and outcomes, thus building upon the near-term data brought to light by the PLATFORM trial.27 To this end, future studies such as the Assessing Diagnostic Value of Non-invasive FFRCT in Coronary carE (ADVANCE) study will investigate the clinical and economic impact of FFRCT as well as the potential reclassification of subjects with abnormal FFRCT for adverse cardiovascular outcomes.23 Determining the appropriate risk factors and CT characteristics for performing FFRCT remains a pressing issue for future research to address. Further, studies aimed at evaluating the cost-effectiveness of FFRCT should be considered. Hlatky et al. investigated the initial treatment costs from 96 patients in the DISCOVER-FLOW trial.31 In this study, the use of FFRCT for guiding the referral of patients for ICA and percutaneous coronary intervention reduced costs by 30 % ($7,674 per patient) when compared with the most commonly used ICA/visual strategy ($10,702 per patient), highlighting the potential value of FFRCT in a clinical setting.
The performance of ‘virtual stenting’ is an emerging topic in the field of FFRCT. In this regard, the computational modelling required for FFRCT allows for the modification of coronary flow models. Moreover, Kim and colleagues documented a positive correlation between invasive FFR and FFRCT before and after stenting, while displaying a 96 % overall accuracy.32 In that study, the investigators demonstrated the feasibility of virtual coronary stenting of CT-derived computational models, suggesting this technology may prove useful for predicting functional outcomes after coronary revascularisation.
Conclusion
FFRCT is a novel non-invasive technique for determining the haemodynamic significance of coronary artery stenosis. Prospective advances in FFRCT technology will assist in overcoming some of the current considerations associated with FFRCT. On-going prospective studies designed to compare the diagnostic power of FFRCT with other stress imaging tests will also offer clinicians an evidence-based alternative for detecting significant CAD, allowing for appropriate utilisation of FFRCT in the clinic.







