Aortic stenosis (AS) is the most frequent form of valvular heart disease referred for surgery in Europe and is the second most prevalent form of valvular heart disease in the US.1,2 Conversely, moderate or severe mitral regurgitation (MR) is the most prevalent valvular disease in the US and the second most common form of valvular heart disease requiring surgery in Europe.1,2 AS and MR frequently coexist and the prevalence of both valvular lesions increases with age.2,3 While AS imposes a pressure overload on the left ventricle (LV) leading to LV concentric hypertrophy,4 MR exerts a volume overload leading to progressive LV and LA dilatation.5 Indeed, severe AS may create or even worsen MR by increasing the LV to left atrial pressure gradient thereby augmenting the regurgitant volume for any given effective regurgitant orifice.6
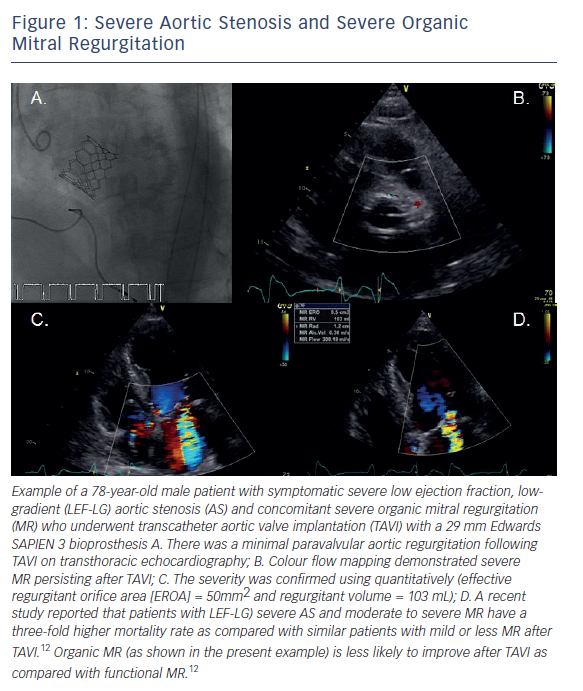
Both valvular lesions can lead to pulmonary hypertension and right ventricular dysfunction in isolation (severe MR more so than severe AS) but the combination of both compound the problem, resulting in hypertrophic remodeling of the pulmonary arterioles and potentially irreversibly elevated pulmonary artery pressures.7 AS is mainly caused by a degenerative inflammatory process, which is typically initiated by mechanical stress of the valve leaflets.4 Conversely, MR aetiology is more heterogeneous and may be categorised as either organic (intrinsic valve lesions) or functional (structurally normal mitral valve but deformation caused by ventricular remodelling).5 Surgical aortic valve replacement (SAVR) has traditionally been considered the gold standard treatment of severe symptomatic AS but up to one-third of patients with symptomatic severe AS are denied treatment owing to advanced age and co-morbidities.1,8 Several randomised clinical trials have demonstrated TAVI to be a non-inferior or even a superior alternative to SAVR in high-risk patients with severe AS.9–11 Moderate or severe MR is present in up to one-third of patients undergoing TAVI and the prevalence is even higher among certain AS subgroups such as patients with low ejection fraction, low-gradient (LEF-LG) severe AS (20–55 %).3,12 In contrast to patients undergoing SAVR, significant MR is generally left untreated among patients assigned to TAVI (see Figure 1).3 The aim of this review is to summarise the data to date regarding the effect of significant (i.e. moderate or severe) MR on clinical outcomes after TAVI.
Mitral Regurgitation Aetiology
Organic MR is the most common aetiology of MR (60–70 %) and is frequently due to primary myxomatous disease, primary flail leaflets or calcification of the mitral valve apparatus.5 Mitral valve prolapse is an abnormal systolic valve movement into the left atrium (≥2 mm beyond the annular level).5 Prolapse can either be moderate (leaflet tips remain in the LV i.e. billowing mitral valve) or severe (eversion of the leaflet tip into left atrium, i.e. flail leaflet).5 The main phenotypes of mitral prolapse are diffuse myxomatous degeneration (Barlows disease) or primary flail leaflets with ruptured chordae, affecting the posterior leaflet in 70 % of cases.5 The presence of a flail leaflet almost always indicates advanced disease and surgery is required even in asymptomatic low-risk patients with preserved LV function and an LV end-systolic diameter ≥40 mm.1,13 Rarer causes of organic MR include endocarditis as well as congenital (cleft leaflet), rheumatic (acute and chronic rheumatic fever), iatrogenic (radiation/drugs) and inflammatory (lupus/anticardiolipin, eosinophilic endocardial disease, endomyocardial fibrosis) conditions.5 While organic MR is more prevalent in the general population, functional MR is more prevalent among elderly patients referred for TAVI.3 This may be related to the high prevalence of concomitant coronary artery disease (40–70 %) among severe AS patients undergoing TAVI.14 Functional MR is usually related to ischaemia and is caused by apical and inferiorpapillary- muscle displacement due to ischaemic left-ventricular remodeling.5 Papillary-muscle displacement exerts traction on leaflets because chordae are non-extensible, which results in tethered and apically displaced leaflets (tenting). Together with annular flattening, enlargement and decreased contraction, mitral valve tenting results in coaptation loss that results in functional MR.5
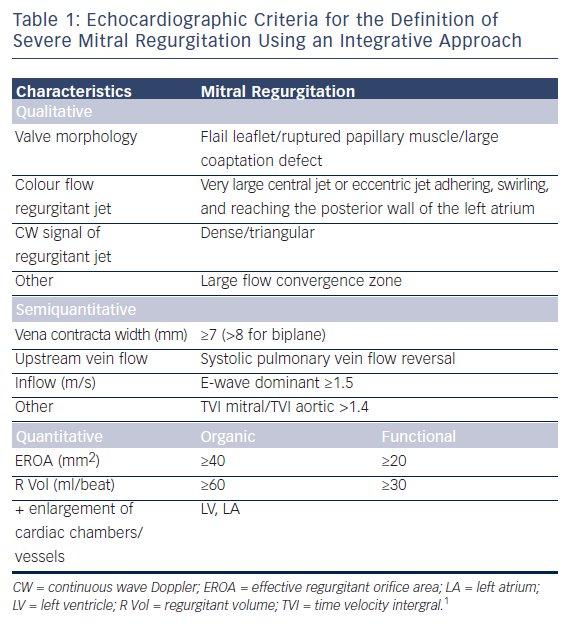
It should be noted that ischaemic MR is not synonymous with functional MR since ischaemic papillary muscle rupture is classified as organic MR. Non-ischaemic causes of functional MR include cardiomyopathy, myocarditis and other non-ischaemic causes of left ventricular dysfunction.5 Carpentier proposed to classify MR into three types according to leaflet movement: type I (normal movement), type II (excessive movement) and type III (restrictive movement: IIIa – diastolic restriction; IIIb systolic restriction).5 The assessment of MR severity using echocardiography comprises qualitative (e.g. valve morphology, colour flow regurgitant jet, continuous wave signal of regurgitant jet), semiquantitative (e.g. vena contracta width, systolic pulmonary vein flow reversal) and quantitative (e.g. effective regurgitant orifice area [EROA] and regurgitant volume [R Vol]) methods.15 EROA and R vol can be calculated by either the flow convergence or the Doppler volumetric method.15 Severe primary MR is defined quantitatively as an EROA ≥40 mm2 and a R vol ≥60 ml.1,15 In secondary MR, lower thresholds of severity using quantitative methods, have been proposed (EROA ≥20 mm2 and R vol ≥30 ml) because of their prognostic value.1,15
Other criteria for severe MR are shown in Table 1. The assessment of AS severity is more complicated in the presence of significant MR owing to the fact that forward stroke volume is reduced due to the R vol « lost » in the left atrium.6 Mean transaortic gradient is directly proportional to the square of transvalvular flow meaning that even small reductions in stroke volume can result in significant reductions in the pressure gradient.16 This in turn can lead to guideline discordant mean gradient and aortic valve area values making the grading of AS severity challenging among patients with significant MR.
SAVR and Significant MR
Double valve interventions are associated with a higher perioperative mortality rate compared with isolated SAVR.17,18 In the Society for Thoracic Surgeons (STS) registry, the perioperative mortality after double (mitral-aortic) valve intervention was almost three-fold higher (9.4 %) compared with isolated AVR (3.2 %).17,18 The decision to intervene on the mitral valve in the setting of severe AS depends on the severity and the aetiology of MR. In symptomatic patients with severe AS, valve replacement (conventional or percutaneous) is the treatment of choice, while in patients with severe MR, valve repair is generally favoured over replacement if feasible especially among patients with organic disease.4,5 This is mainly due to the fact that mitral valve repair is associated with lower perioperative mortality, improved survival and better preservation of post-operative LV function.1,19
For example, in the STS registry, perioperative mortality was 5.7 % for mitral valve replacement versus just 1.6 % for mitral valve repair.17 Conversely, among patients with severe functional MR of ischaemic aetiology, there appears to be no clear benefit of mitral valve repair over replacement, despite indications from earlier retrospective studies suggesting there was.20,21 A recent multicentre randomised clinical trial revealed no significant differences in left ventricular reverse remodeling or survival at 2 years among patients randomised to repair versus replacement.21 MR recurred more frequently in the repair group, leading to more heart-failure-related adverse events and cardiovascular admissions.21 Whether these results can be extrapolated to patients with severe functional MR undergoing SAVR is uncertain. Among patients undergoing SAVR there is a general consensus that a double-valve operation is indicated in the presence of severe MR.5 The management of moderate MR at the time of SAVR is controversial.22–24
A recent meta-analysis suggested that moderate MR left untreated during SAVR may be associated with worse early and late clinical outcomes, suggesting that double-valve intervention may be indicated in such instances.22 Barreiro et al. reported a higher mortality rate among patients with moderate MR of mainly organic aetiology (63 %) left untreated at the time of SAVR.23 Among patients with moderate functional MR undergoing SAVR, Ruel et al. observed that untreated moderate functional MR had no independent adverse effect on survival at mean follow-up of 5.4 ± 3.4 years.24 AS patients with moderate functional MR and one additional risk factor (left atrial diameter >5 cm, mean/peak gradient <40/60 mmHg or atrial fibrillation [AF]) were at increased risk for the composite outcome of heart failure symptoms, cardiac death or subsequent mitral repair or replacement (hazard ratio [HR] 2.7; p=0.004).24
In the Placement of Aortic Transcatheter Valve (PARTNER) trial, 59 of the 299 patients who underwent isolated SAVR had moderate (90.5 %) or severe (9.5 %) MR.25 As compared to patients with mild or less MR, overall mortality rate at 2 years was significantly higher among patients with moderate or severe MR (49.1 % versus 27.9 %; p<0.01). In addition, moderate or severe MR was an independent predictor of 2-year mortality in multivariate analysis (HR 1.77; 95 % confidence interval [CI] [1.17–2.68]).25 However, in a recent multicentre clinical trial randomising patients undergoing CABG with moderate functional MR of ischaemic aetiology to either CABG alone or CABG plus mitral-valve repair, the addition of mitral valve repair did not improve LV reverse remodeling as compared with CABG alone and led to more adverse events.26 The prevalence of moderate or severe MR was reduced at 1 year in the repair group and whether or not this may improve outcomes over medium- to long-term follow-up remains to be seen.26
Prevalence of MR in Patients Undergoing TAVI
The prevalence of moderate to severe MR among patients undergoing TAVI ranges between 2–33 % of all patients with severe AS undergoing TAVI, but among certain subgroups, such as patients with LEF-LG severe AS, the prevalence is considerably higher (20–55 %).3,12 Only a few studies have provided data on MR aetiology in patients undergoing TAVI.27–34 While organic MR is usually more frequent than functional MR in the general population, the latter is more common than the former among high-risk patients selected for TAVI.3,5 No study to date has reported the prevalence of mixed MR aetiologies (i.e. organic + functional), but it is likely to be significant.
Effect of MR on Short Term Outcomes After TAVI
There are studies which suggest an increase in early mortality after TAVI among patients with significant MR at baseline27,33,35–37 and other studies that have not observed this association.12,25,38,39 The reasons for the discrepancies are due to the different definitions used to define significant MR, with some studies evaluating severe MR only,35,37 whereas others report the effect of moderate/severe MR on outcomes after TAVI.25,33,36,38,39 Many retrospective studies may be underpowered to detect differences at 30-days owing to relatively low event rates.
Recently three meta-analysis studies have been published assessing the effect of moderate to severe MR on clinical outcomes after TAVI.40–42 First, Nombela-Franco performed a large meta-analysis of eight studies enrolling 8,015 patients (self-expandable valve 43 %, balloonexpandable valve 64 %, 1 % other) assessing the effect of moderate to severe MR on clinical outcomes after TAVI.40 The authors found that overall 30-day mortality rates were significantly increased in patients with moderate-to-severe MR (odds Ratio [OR] 1.49, 95 % CI [1.16–1.92]) although significant heterogeneity was observed across studies (p<0.05).40 While the impact of MR on mortality was not different between self-expandable and balloon-expandable valves in metaregression analysis (p=0.36) significant MR was more likely to improve among patients receiving a balloon expandable valve as compared with a self-expandable valve.40 Several factors were postulated to explain this observation including the possibility that the longer frame of the CoreValve™ system could mechanically interfere with the anterior mitral valve leaflet.30 However, this putative mechanism was not confirmed in a large CoreValve registry.27 The higher prevalence of post-procedural paravalvular aortic regurgitation may maintain volume overload and contribute to less MR improvement in such patients.43,44 Furthermore, CoreValve implantation is associated with a higher rate of both left bundle branch block and permanent pacemaker implantation, which may lead to LV dysynchrony and a negative effect on LV remodeling and consequently less MR improvement.45
Second, Chakravarty et al. performed a meta-analysis of eight studies (three of which were conference abstracts only) enrolling 8,927 patients assessing the impact of moderate to severe MR on outcomes after TAVI.41 The authors observed that mild or less MR was present in 77.8 % and moderate to severe MR in 22.2 % of patients.41 They observed that the presence of moderate to severe MR at baseline was associated with an increased 30-day mortality rate (relative risk [RR] 1.35; 95 % CI [1.14–1.59]; p=0.003) and that the increased mortality associated with moderate-severed MR was not influenced by MR aetiology (p=0.56).41
Finally, Sannino et al. performed a meta-analysis of 13 studies enrolling 4,839 patients undergoing TAVI and observed that all-cause mortality was increased at 30-days after TAVI (effect size -0.18, 95 % CI [-0.31– -0.04]).42
Effect of MR on Mid- to Long-term Outcomes After TAVI
Data from several national registries including the German, Italian, French2 and Spanish TAVI registries observed a significant association between moderate to severe MR and 1 year mortality after TAVI.27,37,46,47 In the French2 and Spanish TAVR registries, there remained only a trend toward higher mortality after adjustment for confounding variables in the multivariate analysis.37,47 Conversely, a post-hoc analysis of the PARTNER Cohort A trial found that moderate to severe MR at baseline did not affect 2-year mortality among TAVI patients (HR 1.14; 95 % CI [0.72–1.78]; p=0.58]), although it did have an impact among patients assigned to SAVR (HR 1.73; 95 % CI [1.01–2.96]; p=0.04).25 Nombela- Franco reported in their meta-analysis that 1-year mortality rates were significantly increased among patients with moderate to severe MR (HR 1.32; 95 % CI [1.12–1.55]) and that the impact of MR on mortality was not different between SEV and BEV in meta-regression analysis (p=0.39).40
In the meta-analysis by Chakravarty et al., a strong association between moderate to severe MR and 1-year mortality after TAVI was observed (RR 1.24; 95 % CI [1.13–1.37]; p<0.0001).41 The investigators observed that moderate to severe residual MR after TAVI was associated with significantly increased one-year mortality (RR 1.48; 95 % CI [1.31–1.68; p<0.00001]).41 Finally, Sannino et al. found that moderate to severe MR was associated with both 1-year (effect size -0.22; 95 % CI [-0.36– -0.08]) and 2-year (effect size -0.15; 95 % CI [-0.27– -0.02]) mortality rates after TAVI in a meta-analysis enrolling 4,839 patients.42 The results were mainly derived from observational studies that were not specifically designed to assess the impact of MR on mortality. Additionally the PARTNER Cohort A & B trials were the only randomised controlled trials included in these metaanalysis and concomitant severe MR was an exclusion criteria in both PARTNER trial cohorts.9,10 There was also significant heterogeneity across studies for mortality outcome.40–42 Furthermore, the aetiology of MR (functional versus organic) was not available in the majority of studies. These are the main limiting factors for the aformentioned meta-analysis studies.
Effect on MR on Clinical Outcomes of Patients with Low Ejection Fraction, Low-gradient Severe AS
Up to one in six patients undergoing TAVI present with LEF-LG severe AS and concomitant MR is present in 30–55 % of these patients.12 A recent study revealed that LEF-LG patients with moderate or severe MR had a three-fold higher rate of overall mortality at one-year (11.5 % versus 38.1 %; adjusted HR 3.27; 95 % CI [1.31–8.15]; p=0.011), as compared with LEF-LG patients with mild or less MR.12 Patients with organic MR had higher one-year mortality rates as compared with those with functional MR (adjusted HR 3.38; 95 % CI [1.32–8.67]; p=0.011).12 However, LEF-LG patients with moderate or severe MR assigned to medical therapy had a dismal prognosis independent of MR severity suggesting that TAVI should not be withheld from symptomatic patients with LEF-LG severe AS even in the presence of moderate or severe MR.12
Changes in MR Severity After TAVI
In patients with severe AS and concomitant significant MR, several physiological changes occur following valve implantation that may contribute to reducing MR severity. The LV systolic pressure drops precipitously after TAVR/SAVR thereby reducing the LV-left atrial pressure gradient, leading to a reduction in MR in many patients. The late regression of concentric LV hypertrophy observed following TAVI due to a decrease in LV afterload can lead to favourable mitral valve haemodynamics.48 Furthermore, changes in LV geometry due to a reduction in LV end-diastolic volume and mitral tethering forces observed after TAVI may also lead to an improvement of functional MR (i.e. reverse remodeling).3 Nombela-Franco et al. observed that moderate to severe MR showed improvement in 51 %, no change in 47 % and worsening in 2 %.40 Reassuringly, MR appears to worsen following TAVI in only a minority of patients (2–7 %). Several studies have assessed predictors for MR improvement after TAVI.
Toggweiler et al. found that an absence of AF, absence of pulmonary hypertension (pulmonary artery systolic pressure [PASP] <60 mmHg), a mean gradient ≥40 mmHg and functional (as opposed to organic) MR were predictors of MR improvement following TAVI. These findings were confirmed by Bedogni et al., who also found that absence of atrial AF, pulmonary hypertension (PASP ≤55 mmHg) and functional MR were predictive of MR improvement after TAVI. Giordana et al. and Nombela-Franco et al. observed that valve type (BEV versus SEV) was a predictor of MR improvement.34,40 Hekimian et al. observed that an LV ejection fraction <50 %, a LV end-systolic diameter ≥36 mm and an LV end-diastolic diameter ≥50 mm were predictors of MR improvement.32 The presence of prosthesis-patient mismatch leads to a residual gradient across the aortic valve and has been shown to be associated with a lesser regression of coexistant MR after SAVR.49–50 TAVI is associated with lower rates of prosthesis-patient mismatch and whether this translates into differences in MR improvement as compared with SAVR remains to be seen.51
Percutaneous Treatment of MR After TAVI
Percutaneous mitral valve repair using the Mitraclip® (Abbot Vascular) is associated with improved outcomes compared with conservative therapy in patients with symptomatic severe MR who are deemed high risk or inoperable.52 TAVI patients who remain symptomatic due to significant MR could potentially profit from a staged percutaneous procedure to treat MR. This may be a particularly attractive option for the sub-set of patients with LEF-LG severe AS and moderate to severe MR, who tend to have a particularly high mortality after TAVI. The first description of Mitraclip device being inserted as a staged procedure after TAVI with the Edwards and CoreValve devices was in 2011.53,54 The aortic valve bioprothesis did not seem to interfere with Mitraclip implantation. There is a lack of evidence on the clinical benefits associated with this procedure in the TAVI patient population. However it seems to be technically feasible and it may be a low-risk therapeutic option for patients with significant MR who remain symptomatic after TAVI.
Management Strategy of Patients with Significant MR Undergoing TAVI
The management strategy of patients with severe AS and concomitant moderate or severe MR depends on a number of factors including operative risk, MR severity, MR aetiology and likelihood of improvement. Key to decision-making is the evaluation of MR aetiology and severity by quantitative echocardiographic methods, with the use of transoesophageal echocardiography if necessary. Among low or intermediate risk patients with moderate or severe MR, patient selection is critical to identify patients in whom MR will not improve or even progress after SAVR. In such patients with a low likelihood of MR improvement (e.g. patients with severe MR due to a flail leaflet) the increased risk of a double-valve procedure may be worthwhile. Among high risk patients in whom both SAVR and TAVI are options, identification of factors associated with improvement may lead one to choose one procedure over another. Therefore, patients with a high likelihood of MR improvement after the intervention (e.g. patients with low ejection fraction and functional MR) might be selected to undergo TAVI, whereas a combined SAVR and mitral valve repair or replacement may be a more attractive option in patients with a low chance of MR improvement after TAVI. Among inoperable patients, TAVI is the best option if feasible, especially among patients with concomitant MR of functional aetiology. Among inoperable patients who remain symptomatic due to severe MR even after TAVI, percutaneous repair of the mitral valve could be considered, although data remain scarce regarding the feasibility of this approach.53–56
Conclusion
Moderate to severe MR is commonly present among patients selected to undergo TAVI and is associated with an increased risk of both early and late mortality after TAVI. However, because of the limitations of the data hitherto available, it is not clear whether this association is related to the MR severity or whether MR is simply a marker of a worse prognosis. Patients with significant MR tend to have worse baseline characteristics including poorer LV function and it may not be possible to adjust for all confounders. MR severity typically improves after TAVI in about half of patients and worsens in only a small minority of patients. In the remaining patients, MR severity remains the same. Future study areas include randomised controlled clinical trials assessing the feasibility of percutaneous management of concomitant moderate to severe MR versus medical management among patients undergoing TAVI. Such studies will require centralised core laboratories to define the precise mechanism and severity of MR using quantitative methods and standardied methods of grading MR severity.