Vulnerable atherosclerotic plaque comprises a lipid-rich necrotic core, covered by a thin fibrous cap, that is weakened by macrophage infiltration.1 Plaques that have this morphology and composition have a greater probability of being associated with acute coronary syndromes in clinical studies.2,3 Coronary artery disease is most commonly triggered by the rupture of vulnerable plaque and thrombosis.4 The identification of vulnerable plaque is emerging as an important element in coronary artery disease diagnosis and treatment.
In the past three decades, several imaging modalities have been employed to identify vulnerable plaque. Coronary angiography is the oldest of these modalities and can only visualise the artery lumen, not the artery wall and atherosclerotic lesions. Moreover, angiography creates images of a three-dimensional moving object that are presented in a two-dimensional plane. Intravascular, catheter-based imaging methods can be safely used in a routine catheterisation laboratory population5 and offer direct visualisation of the artery wall. Intravascular ultrasound (IVUS) imaging has been used in routine clinical practice for more than 20 years. Due to the limited acoustic contrast between soft tissues, the conventional grayscale IVUS image is not sensitive enough to differentiate plaque composition, except for the presence of calcium.6,7 While the application of an advanced analysis algorithm to IVUS images – virtual histology IVUS – has improved plaque composition characterisation,8 no data yet support its accuracy in the detection of lipid-rich necrotic plaque core.9–11 IVUS palpography is a technology used to assess local mechanical plaque properties based on tissue deformation caused by intraluminal pressure.12 It can only sense the stiffness of the tissue, however, and cannot directly image the tissue, and it only assesses the first 450 μm of the arterial wall.12 Light-based intravascular optical coherence tomography (IVOCT) creates high-resolution images (approximately 15 μm) with backscattered light from the tissue13 and can image plaque components such as calcium, lipid and thrombus. IVOCT currently relies on qualitative image interpretation to distinguish these features.14,15 The depth to which IVOCT penetrates is only 1–2 mm into the atherosclerotic tissue, which means it often cannot see the extent of the plaque up to the adventitia. Near-infrared spectroscopy (NIRS) is another light-based imaging modality for the detection of lipid-rich necrotic core in plaque.16 It provides a probability for the presence of coronary lipid based on the spectral analysis of backscattered light;17 however, NIRS cannot identify the amount and location of lipids, which may be important in risk assessment.18
Several other innovative optical modalities have been proposed recently19–22 that are currently being evaluated in clinical trials. The ability of these technologies to provide reliable, spatially-precise, quantitative imaging of plaque lipid content is yet to be determined. In this paper, a newer modality is reviewed: intravascular photoacoustic (IVPA) imaging. This is an optical–acoustic hybrid imaging modality. IVPA is currently being developed to show both the morphology and chemical composition of the artery wall with a good imaging depth and resolution. This technology takes advantage of the unique optical absorption contrast between different tissues and reasonably large penetration depth owing to the low acoustic attenuation in soft tissues.23,24 Published experimental data suggest it may be a strong contender for detailed plaque characterisation and the identification of plaque at increased risk of causing clinical sequelae.
The Principles of IVPA Imaging of Atherosclerotic Plaque
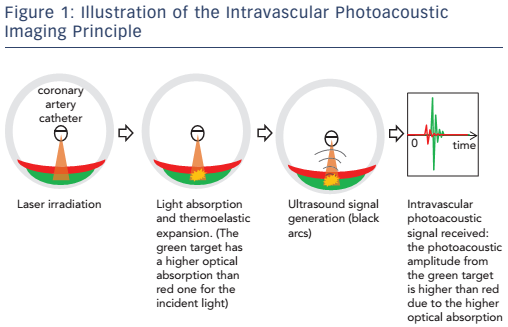
IVPA imaging requires short laser pulses, lasting a few nanoseconds, to be applied to irradiate the artery wall. Absorption of the light converts the optical energy into heat in the tissue and causes thermoelastic expansion, leading to a transient pressure rise (the laser pulse duration is shorter than both the stress relaxation and the thermal diffusion times). Figure 1 illustrates the principles involved in IVPA imaging.
The specific optical absorption spectra of lipids and other pure substances can be related to the identification of plaque.25 Various biomarkers present in plaques have been explored for their usefulness in IVPA imaging, with lipid being the most frequently used. IVPA imaging of plaque lipids can be performed at around 1.2 μm or 1.72 μm due to the high lipid-specific absorption contrast with relatively high resolution (~50 μm) and reasonable penetration depth.26 At 1.2 μm the laser’s maximal permissible exposure limit is 20 mJ/cm 2 and at 1.72 μm it is 1 J/cm 2, according to the American National Standards Institute laser safety standard.27,28 NIRS also makes use of lipid to identify potentially vulnerable plaque, but there is no depth resolution. The capability of IVPA to produce images of atherosclerotic plaque lipids has been demonstrated extensively with ex vivo tissues and in vivo animal models.26,27,29–33
Macrophages are an important cell type related to the progression of atherosclerosis34 and the specific imaging of plaque macrophage content is a potentially interesting feature when identifying vulnerable plaque.36 Macrophages do not exhibit a strong intrinsic contrast in the way lipids do, therefore exogenous imaging contrast agents with high optical absorption are applied in order to visualise them using IVPA imaging.36,37 Furthermore, given that the activity of the enzyme matrix metalloproteinase (MMP) is an indicator of plaque instability, the localisation of MMP activity with an MMP-sensitive activatable probe in vulnerable plaques in human carotid specimens has been achieved using photoacoustic imaging.38 More recently, an ApoE-/- mouse in vivo model injected with a photoacoustic ICG@PEG-Ag2S nanoprobe was successful in imaging plaque.39
Developing IVPA Imaging for Clinical Use
Encouraged by the capability of IVPA to create images of vulnerable atherosclerotic plaque, an intensive research effort is on-going to incorporate IVPA imaging into clinical applications.
Miniaturising the IVPA Catheter
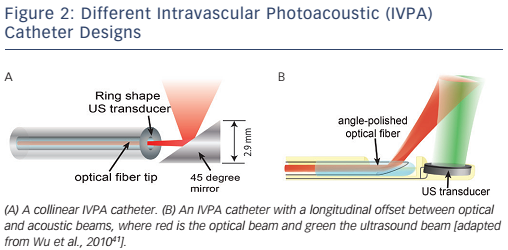
A miniature, and highly sensitive, catheter for IVPA imaging is an essential element if IVPA imaging technology is to enter common use. As IVPA is an intrinsically multimodal imaging technique, the catheter’s technical requirements are harder to meet than for single-modality probes like optical coherence tomography or IVUS catheters. A typical IVPA imaging catheter consists of an optical part for light delivery and a broadband ultrasound transducer. The optical part is usually a combination of an optical fibre and a mirror or a single-angle polished optical fibre.40 Two IVPA catheter designs are shown in Figure 2. The unit shown in Figure 2A provides the greatest reported sensitivity. Miniaturisation is challenging, however, and this unit is currently too large for intravascular application, having a diameter of 2.9 mm.27,28 Another design possibility – one that is favoured for miniaturisation – incorporates an offset between the optical fibre and ultrasound transducer, either longitudinally41,42 (see Figure 2B) or laterally.43 The smallest IVPA catheter reported to date that uses this design has an outer diameter of 0.9 mm, which is below the threshold of 1 mm desired for clinical translation into coronary arteries.44
Efficient and Specific Plaque Identification
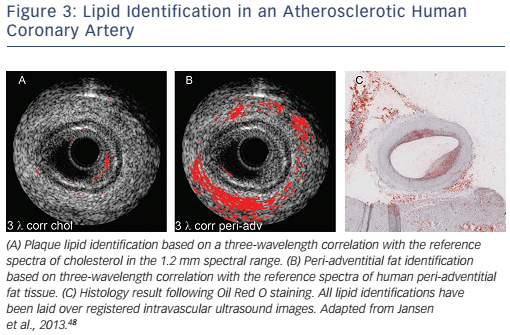
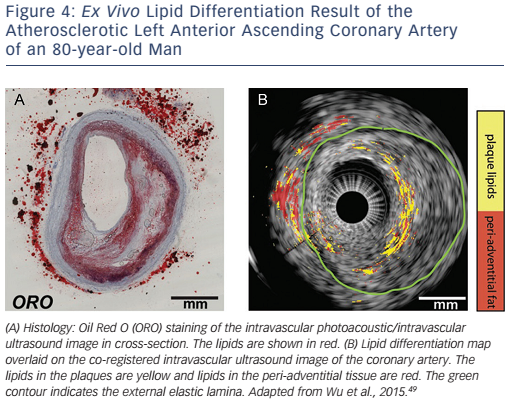
Lipids are found in the plaque inside the artery wall, which is rich in cholesterol and cholesteryl esters,45,46 as well as in peri-adventitial fat tissue around the artery, which contains a mixture of fatty acids.47 The spectral contrast between plaque lipids and peri-adventitial fat makes it possible to differentiate between them using spectroscopic IVPA imaging (sIVPA).26 As a consequence of this, the presence and location of lipids within a plaque can be reliably and rapidly displayed during catheter pullback, using both cross-sectional and longitudinal data display. Performing multiple wavelength sIVPA imaging, however, has an impact on the complexity, cost andspeed of the imaging system. Minimisation of the number of wavelengths for the differentiation of different lipids or improving the efficiency for specific lipid differentiation is necessary for practical application. The possibility of specific plaque lipid imaging using sIVPA with limited number of wavelengths has been investigated (see Figure 3).26,48 It is possible to achieve about 70 % true positive and 15 % false positive pixel identification of plaque lipids based on the relative difference between amplitudes of only two wavelengths (see Figure 4).49
High-speed IVPA Imaging of Atherosclerotic Plaque
Despite successful plaque identification by IVPA imaging, the low imaging speed limits its application in practice. Lipid specificity remains limited by the single-wavelength operation and the average optical power remains quite high (up to 1 W), which raises concerns about thermal damage to the patient’s artery and the potential hazard to the operator resulting from skin and eye exposure. With the introduction of higher pulse-rate laser systems (2 kHz), IVPA imaging speed has been increased from about 0.3 to 1 frame per second.27,28,50 This represents a significant step forward, but is still not practical. More and faster IVPA imaging systems are, however, on the horizon. A fast multiplewavelength sIVPA imaging system with potentially ~5 frames per second has been developed that is capable of imaging at a low-energy pulse.44
Discussion
IVPA imaging shows great promise in detecting the morphology and composition (e.g. lipid deposition) of arterial lipid plaque burden. Owing to the extensive research on IVPA imaging, several important milestones have been passed, with the development of a miniature flexible catheter (<1 mm in diameter), high-efficiency specific imaging of vulnerable plaque composition and the development of a highspeed IVPA imaging system (~ 5 frames per second). Some challenges remain, however, in the further development of IVPA imaging.
Most current IVPA imaging systems require the artery to be cleared of blood by flushing for a better photoacoustic signal-to-noise ratio. It is in principle possible to perform IVPA imaging at 1.72 μm without flushing, due to the similarity in the optical absorption property of blood and water-based tissues. Wang et al. performed the first in vivo IVPA imaging (at 1,720 nm) in a hypercholesterolemic rabbit model through blood.29 Further IVPA imaging through blood – and in and ex vivo human tests – must await the resolution of other clinical implementation issues described in this article. Although the imaging speed has been significantly improved,51–53 it is still not fast enough for clinical use. Recently, it was found that the sensitivity of IVPA catheters can be increased by an order of magnitude by matching the frequency response of the receiving transducer to the low-frequency range.54,55 This enables imaging with lower pulse energy, allowing for fast laser sources with moderate output power. Other challenges in adapting IVPA imaging to the clinical setting include the cost and robustness of the laser system and the choice of catheter sheath material, which needs to be transparent for ultrasound and infrared light. These topics being investigated in on-going engineering research.
Conclusion
IVPA imaging is unique in its biochemical specificity and can offer the clinician direct, validated visualisation of coronary plaque lipid. To many clinicians, the ideal tool for guiding atherosclerotic plaque diagnosis and interventions requires high resolution to characterise the thin cap, high sensitivity to detect lipids for plaque visualisation in the artery, and a reasonable depth of penetration for plaque burden assessment. To achieve this, the combination of IVOCT and IVPA appears to be a promising choice, but at the cost of integrating an extra optical coherence tomography laser system. However, the natural progression of plaque with vulnerable characteristics is complex and the development and application of clinical tools for its assessment is, likewise, challenging. To date, IVPA imaging remains a research tool; future advances in technology will determine to what degree it will be of use in clinical practice.