Dr Soltesz discussed how he and his team at the Cleveland Clinic are using Impella 5.5 to support patients who are at high risk for heart surgery. Many high-risk cases are denied surgery due to significant risk of postoperative mortality. Furthermore, many patients who do undergo surgery still require salvage support due to post-cardiotomy cardiogenic shock (PCCS); however, these therapies come with their own significant drawbacks and risks. For example, the intra-aortic balloon pump (IABP) offers minimal support while requiring the patient to be bed-bound and intubated for a prolonged period, and extracorporeal membrane oxygenation (ECMO) also renders the patient bed-bound and intubated while providing poor unloading and a risk of bleeding. As such, some patients are being directly referred to advanced therapies, such as durable left ventricular assist devices.
The Coronary Artery Surgery Study (CASS) trial, which compared the medical and surgical treatment of patients with chronic, stable coronary artery disease, revealed that coronary artery bypass graft (CABG) surgery is demonstrably effective for patients with left ventricular failure.1 Similarly, the Surgical Treatment for Ischemic Heart Failure (STITCH) trial, which investigated the effect of combining CABG with medical therapy in heart failure patients, demonstrated that, in patients with ischaemic cardiomyopathy, CABG results in a 21% reduction of death from cardiovascular causes at the 10-year follow-up.2 Dr Soltesz noted that although long-term survival was significantly increased, the risk of death is higher in the first 30 days, suggesting that therapies need to be focused on getting patients through that early hazardous period to reap the long-term benefits. Most early mortalities are due to PCCS, which occurs in 0.2–9% of cardiac surgeries, is difficult to predict and carries a high mortality rate, ranging from 10% to 75%.3,4 Of note, low ejection fraction, high-dose inotropes and long cardiopulmonary bypass (CPB) times are associated with increased risk.
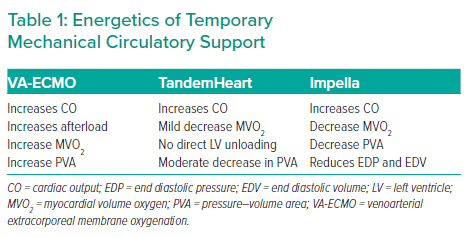
The primary goal of pericardiotomy assist is to unload the injured ventricle, followed by weaning toxic levels of pressors while maintaining end-organ perfusion and function. At the molecular level, this enables cytokine metabolism and ATP store replenishment, allowing the myocardium to recover. Conventional therapies include vasopressors, inotropes, IABP and venoarterial (VA-) ECMO. Vasopressors and inotropes may not be ideal, because they increase myocardial oxygen consumption and stress the myocardium. IABP offers only a slight reduction in pressure–volume area and increased coronary perfusion, whereas VA-ECMO supports systemic perfusion but is costly in terms of myocardial energetics. Dr Soltesz emphasised that unloading is the key to decreasing the chances of poor outcomes for patients at high risk for CABG. Comparisons of different temporary mechanical circulatory supports (MCS), VA-ECMO, TandemHeart and Impella, clearly reveal that Impella provides the best unloading while setting the stage for end-organ recovery (Table 1).
The key to avoiding PCCS is to anticipate it, by performing risk stratification, prehabilitation, planning a temporary MCS and identifying an exit strategy.
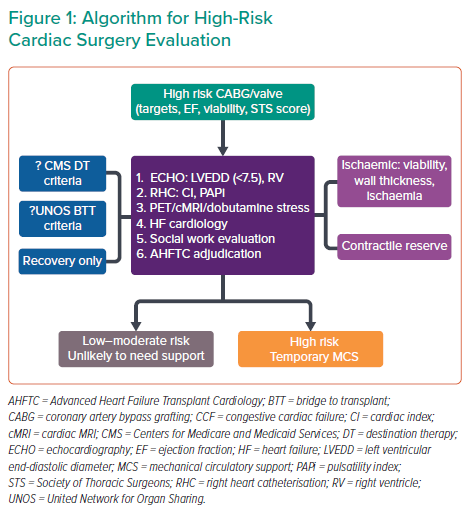
Defining surgical risk requires consideration of numerous patient factors, as well the quality of the coronary target and the viability of the myocardium. Prehabilitation may include Swan-guided therapy, hepatic decongestion, inotropes and/or vasodilator therapy, and possibly preoperative IABP or temporary MCS. At the Cleveland Clinic, risk evaluation is conducted in a stepwise fashion (Figure 1).
Dr Soltesz walked the audience through a case to demonstrate the evaluation system, where a high-risk patient was identified and subsequently treated with CABG and Impella with successful outcomes. Ultimately, the key to success in treating these high-risk patients is both the pre- and intra-operative treatment considerations, which requires assessing the patient thoroughly and providing the best support to reduce mortality risks.
Dr Soltesz concluded that PCCS can be mitigated by minimising CPB time and rapidly escalating the preplanned temporary MCS; pre-emptive use of a pump such as Impella allows left ventricular unloading and improved postoperative recovery. With their algorithm, Dr Soltesz and his team at the Cleveland Clinic have seen improved outcomes with cardiac surgery in properly identified high-risk patients. Defining risk and an exit strategy are key to success.