Background: Studies among very elderly Filipinos with acute ST-elevation MI (STEMI) are limited.
Aim: To determine the clinical profile, treatment strategies and predictors of in-hospital outcome on Filipino octogenarians.
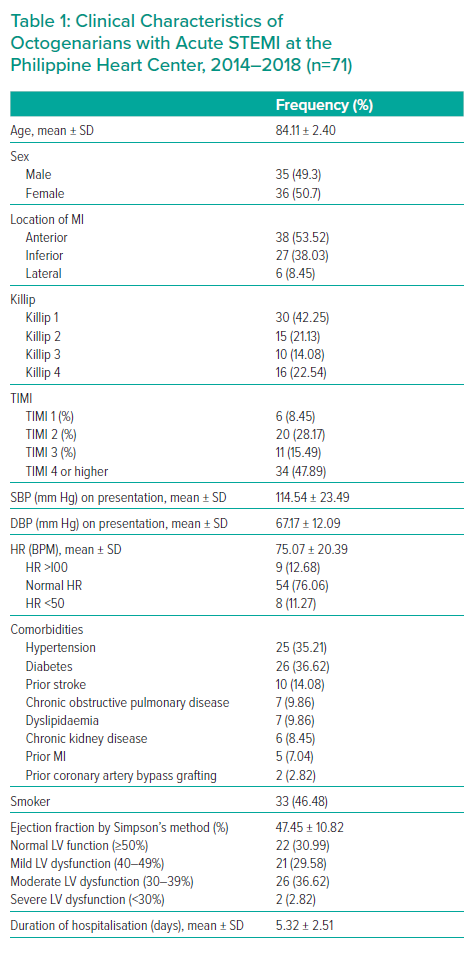
Methods: A retrospective cross-sectional study was conducted at the Philippine Heart Center on all patients who were 80 to 89 years old with acute ST-elevation myocardial infarction (STEMI) from 1 January 2014 to 31 December 2018. Predictors of major adverse cardiovascular events (MACE) and/or in-hospital mortality were determined using binary logistic regression analysis.
Results: There were 71 octogenarians in our cohort with a mean age of 84.11 ± 2.40 years. The most common infarct location was the anterior wall (53.52%). Primary PCI (PPCI) was the reperfusion therapy of choice in 47 octogenarians with angiographic success achieved in 43 cases. There were five patients who expired in the PPCI group. Among the 21 patients who were managed conservatively, 12 expired. Fibrinolysis was performed in only three cases. Cardiogenic shock was the most common major adverse cardiovascular event (MACE) (18, 25.35%). The mean ejection fraction (EF) of our cohort was 47.45 ± 10.82%. A higher EF was associated with a lower risk of developing MACE and/or in-hospital mortality (OR 0.91, p=0.008). Killip Class 4 (OR 8.32, p=0.034), two/three-vessel involvement (OR 2.77, p=0.008) and contrast-induced acute kidney injury (CI-AKI) (OR 6.39, p=0.015) were associated with a higher risk of developing MACE and/or in-hospital mortality.
Conclusion: Octogenarians who underwent PPCI had better outcomes compared to those who were managed medically. A higher ejection fraction was associated with a lower risk of MACE and/or in-hospital mortality. Killip Class 4, multivessel involvement and CI-AKI were independent predictors of MACE and/or in-hospital mortality.