The management of patients with acute ST-elevation myocardial infarction (STEMI) relies on restoring blood flow to the occluded infarct artery. Prompt percutaneous coronary intervention (PCI) and stenting of the stenosis causing the occlusion reduces the risk of cardiac death and recurrent infarction.1 In about half of patients,2 stenoses are identified in non-infarct arteries at the time of the PCI, leading some operators to extend the procedure and carry out an immediate ‘preventive PCI’ in the non- infarct arteries, on the basis that this may prevent future serious cardiac events. Until recently, however, clinical guidelines recommended that PCI be limited to the infarct artery, because of concern that the benefit of preventive PCI may not outweigh the risks of the extended procedure.3,4
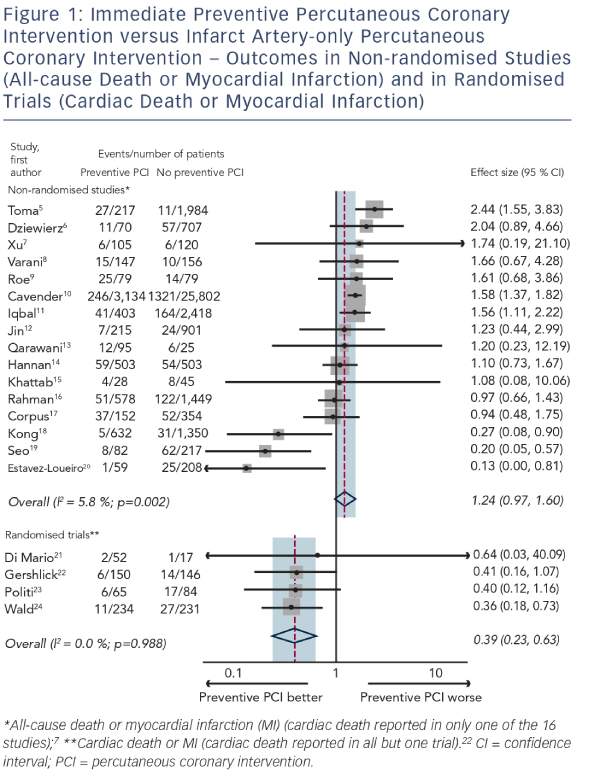
This recommendation was based on non- randomised studies in which the outcome of patients with STEMI and multivessel disease who received immediate preventive PCI at the time of their infarct artery PCI was compared with the outcome of patients treated by infarct artery PCI alone. In these studies, doctors determined who received preventive PCI and who did not. Figure 1 shows a metaanalysis plot of 16 such studies (42,817 patients, median follow-up 12 months).5–20 The summary estimate in the non-randomised studies is not statistically significant but suggests a possible increased risk of all-cause death or non-fatal MI in the preventive PCI group (odds ratio 1.24, 95 % confidence interval [CI] 0.97–1.60; p=0.085). The use of all-cause rather than cardiac death as an outcome is a limitation, because it includes non-cardiac causes that are not influenced by PCI (e.g. cancer) and dilutes the relevant cardiac outcomes, but only one study7 reported cause-specific death. A more serious limitation, in the non-randomised studies, is selection bias: the extent to which patients who received preventive PCI, for example, were sicker than those receiving infarct artery-only PCI and were therefore heading for a worse outcome regardless of the treatment strategy adopted. Selection bias is not avoided by increasing study size or by adjusting for confounding, because not all confounding factors are measured or known, so even in large propensity score-matched studies11,14 it is not possible to be sure which treatment is better. Selection bias is avoided in a randomised trial, since the use of preventive PCI is determined by random allocation rather than physician choice. Four such trials (979 patients, median follow-up 18 months),21–24 in which cardiac deaths were reported in all but one23, have been completed and a meta-analysis plot of these trials is also shown in Figure 1. The relative risk of cardiac death or non-fatal MI is 0.39 (95 % CI 0.23–0.69; p<0.001), showing that selection bias is an important source of error in the non-randomised studies and indicating that preventive PCI, performed as an immediate extension of the infarct artery PCI, reduces the risk of cardiac death and MI by about 60 %.
How can these findings be reconciled with the view that PCI improves symptoms but not prognosis?25–27 The value of angioplasty has been studied in different groups of patients with coronary artery disease. The evidence of benefit in reducing the risk of cardiac death and MI in patients with STEMI is known.1 In patients with non-STEMI, there is a short-term hazard but a long-term benefit.28 In patients with stable angina, prior studies have shown no evidence of prognostic benefit.26–27 This gradation of effect may, at least in part, be due to the fact that PCI causes adverse cardiac events as well as preventing them, and in a lower-risk group, for example, in patients with angina rather than a MI, the benefit may not outweigh the harm.
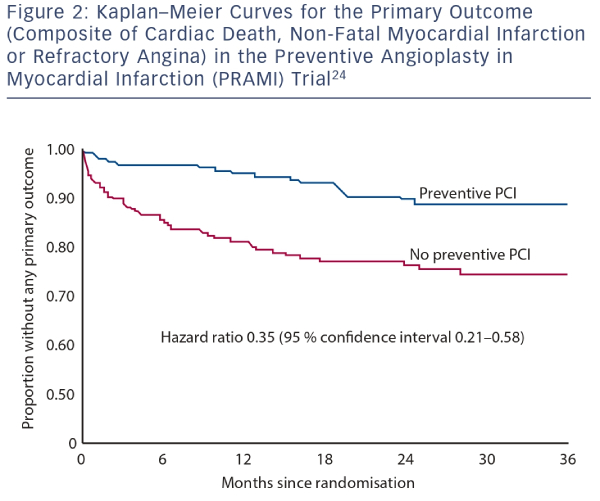
In patients with STEMI, coronary artery plaque rupture remote from the infarct artery has been demonstrated in autopsy29,30 and intravascular ultrasound studies,31–34 which suggess that plaque instability is not a localised vascular event but a generalised process throughout the coronary tree. In an angiographic study of 253 patients with STEMI, the finding of multiple complex coronary artery lesions (>50 % stenosis) remote from the infarct artery was associated with a 10.6-fold excess risk of recurrent acute coronary syndrome within 1 year.35 The simplest, albeit speculative, explanation for the preventive benefit of PCI in such patients is by stabilising plaques prone to rupture and spontaneous thrombosis,36 so reducing subsequent infarction. There is uncertainty whether the benefit outweighs the risk of PCI in stenoses <50 %, since these were not included in the randomised trials. Preventive PCI may also reduce ischaemia by improving coronary flow in severe stenoses and by preventing progression over time, explaining the observed reduction in refractory angina. The concordance between the components of the primary outcomes in Preventive Angioplasty in Myocardial Infarction (PRAMI) (hazard ratios 0.34 [0.11–1.08], 0.32 [0.13–0.75] and 0.35 [0.18–0.69] for cardiac death, non-fatal myocardial infarction and refractory angina, respectively)24 suggests that both mechanisms may be similarly important in the prevention of future cardiac events.
In the PRAMI trial the evidence of benefit emerged early on.24 The curves in the Kaplan–Meier plot (see Figure 2) diverged within a few days and the maximum effect was evident within a few months, suggesting that the immediacy of preventive PCI is important and that staged preventive PCI (undertaken after a few weeks) may not be as effective. The same observations were apparent in the Complete Versus culprit-Lesion only PRimary PCI Trial (CVLPRIT) trial22 in which all but about a quarter of patients in the preventive PCI group had immediate preventive PCI, the remainder having a staged procedure within a few days. Neither of the two trials was designed to compare immediate versus staged preventive PCI. Such a trial, if judged necessary, would need to be large to demonstrate a difference in outcome on top of the 60 % reduction in cardiac death or MI from preventive PCI alone.
The results of PRAMI24 and CvLPRIT22 have prompted a rethink in the way we manage non-infarct artery stenoses in STEMI. The European Revascularisation Guidelines were recently changed (September 2014) and now recommend that immediate preventive PCI be considered in selected patients with STEMI,37 but do not indicate how this selection should be made. The use of a physiological measure of blood flow, such as fractional flow reserve (FFR), may be better than visual angiographic assessment in guiding preventive PCI,38 but it may also worsen outcomes if non-flow limiting stenoses are left untreated and become the sites of future infarction. Three trials of preventive PCI in patients with STEMI are in progress that are using FFR to decide which non-infarct artery stenoses to treat.39–41 No trial is designed to directly compare FFR with angiography in STEMI to determine which, if either, is better in guiding preventive PCI. Further research would be needed to resolve this uncertainty.
A limitation of the trials of preventive PCI, as in all randomised trials, is that they only provide an average effect of treatment. Some patients will benefit more from preventive PCI than others, but in the absence of knowing who they are, no special selection can be recommended. The trials excluded patients with cardiogenic shock, previous coronary artery bypass graft (CABG), significant stenosis of the left main stem or in whom the only non-infarct artery disease was a chronic total occlusion. Therefore, while the benefits of preventive PCI may apply in these selected groups, there is uncertainty. In others, for whom the non-infarct artery stenoses are judged treatable by PCI, the evidence from the trials completed so far, is clear – that immediate preventive PCI confers substantial clinical benefit. The primacy of randomised trials reveals the danger of using non-randomised studies, which can, as in this case, give the wrong answer.







