Coronary chronic total occlusions (CTOs) are common and found in up to 25% of patients undergoing coronary angiography; they are the most challenging lesion subset to treat with percutaneous coronary intervention (PCI).1 A CTO is defined as a completely occluded epicardial coronary artery with thrombolysis in MI (TIMI) flow grade 0, with an estimated duration of at least 3 months.2,3 The presence of a CTO is a significant predictor of incomplete revascularisation.4 In the UK, CTO PCI accounts for approximately 11% of total PCI procedures for stable chronic coronary syndromes, a figure that has remained stable in recent years.5
CTO PCI is associated with lower procedural success than non-CTO PCI and confers a higher risk of complications due to anatomical complexity and the more risky procedural techniques employed.6
The indication for CTO PCI continues to be debated, driven in part by the misconception that non-infarcted myocardium that is supplied by a CTO is not prone to ischaemia due to the presence of collaterals, and because of a lack of convincing randomised data demonstrating a reduction in major adverse cardiovascular events (MACE). However, there is data clearly demonstrating the presence of myocardial ischaemia in regions supplied by a CTO vessel despite extensive collateralisation, and a reduction in ischaemia after successful percutaneous revascularisation.7,8
Successful recanalisation of a CTO has been associated with improved quality of life, reduced angina, improved left ventricular ejection fraction, electrical stabilisation and a reduction in arrhythmic burden, although the impact of elective CTO PCI on survival continues to be subject to debate.9–11 The 2018 European Society of Cardiology/European Association of Cardiothoracic Surgery guidelines on myocardial revascularisation by CTO PCI carry a class IIA/level of evidence B recommendation in patients with ongoing angina refractory to medical therapy or in those with a large burden of ischaemia in the territory of the occluded vessel.12
Due to the complexity and the higher risk associated with CTO PCI, historically CTO intervention has been undertaken only in centres with on-site cardiothoracic surgical back-up, with overnight stays common after the procedure.13–17 The development of advanced CTO PCI equipment and techniques has resulted in improved procedural success and lower complication rates in experienced hands. Nonetheless, the benefit:risk ratio for CTO PCI is less favourable than for PCI in non-CTO lesions and, as a result, it has been suggested that CTO PCI should be performed only in hospitals with on-site surgical back-up.18
To the best of our knowledge, there are no published data regarding the safety and efficacy of CTO PCI in non-surgical centres (NSCs). The aim of this study was to evaluate the feasibility, safety and success of a dedicated CTO programme in a large UK PCI centre with no on-site surgical back-up, as well as the long-term clinical outcomes.
Methods
Portsmouth Hospitals University NHS Trust is a large acute trust with 1,200 inpatient beds. Approximately 1,400 PCI procedures are performed annually across the spectrum of coronary artery disease presentations. Cardiothoracic surgical cover is provided by the regional centre, which is 32.2 km away.
We retrospectively analysed the prospectively collected data for consecutive unselected CTO procedures performed in our unit from January 2015 to December 2019. During the study period, there was one dedicated CTO operator trained in hybrid approaches (AD) as part of the wider six-strong interventional cardiologists undertaking PCI in the unit. In the latter stages of the study period, a second PCI operator was being trained in CTO PCI (BA) and cases were performed jointly as two-operator procedures. In general, less complex CTOs (J-CTO [Multicentre CTO Registry in Japan] score 0–1) were initially attempted by all interventional cardiologists, with more complex cases and procedural failures subsequently referred to the CTO team.
Intervention
CTO PCI was performed using standard techniques via radial and/or femoral arterial access. When CTO PCI was attempted by non-CTO operators, antegrade wiring was the sole strategy used. CTO PCI undertaken by the dedicated CTO team was performed according to the hybrid algorithm, using in addition to antegrade wiring, dissection and re-entry and retrograde approaches.19,20
Data for all CTO procedures undertaken between January 2015 and December 2019 were prospectively recorded using the British Cardiovascular Intervention Society (BCIS) and National Institute for Cardiovascular Outcomes Research database, which lists more than 100 unique variables including patient demographics and risk-factor profiles, technical aspects of the PCI procedure and in-hospital MACE.21
All clinical data, baseline angiograms and procedural characteristics of the CTO procedures were analysed in detail by two experienced operators to assess whether CTO diagnostic criteria were met.
Additional patient characteristics and long-term follow-up data were obtained retrospectively from electronic patient records. Procedural outcomes and in-hospital complications were recorded prospectively and were adjudicated based on the CTO academic research consortium (CTO-ARC) consensus recommendations.3
Endpoints
The main outcomes of interest in this study were the rate of successful revascularisation of CTOs in our unit, the occurrence of procedure-related complications, the requirement for emergency bailout surgery and the rate of in-hospital MACE. We also report long-term outcomes at the longest follow-up time available.
Technical success was defined as achievement of TIMI grade 2 or greater antegrade flow in all ≥2.5 mm distal branches with <30% residual stenosis of the target CTO lesion at the end of the procedure. Procedural success was defined as technical success in the absence of in-hospital MACE. Patient success was defined as final successful disobliteration of a CTO in more than one attempt, following an initial unsuccessful attempt and/or subintimal modification (investment procedure) followed by a planned staged procedure to complete and optimise CTO PCI. Peri-procedural MI was defined according to the fourth universal definition of MI and procedural complications reported as per the CTO-ARC definitions.
However, we did not routinely collect pre- or post-procedural blood samples for measurement of cardiac biomarkers unless clinically indicated (chest pain and/or ECG changes), particularly as the majority of CTO procedures in elective patients were performed as day-case procedures with same-day discharge.
In-hospital MACE included any of the following adverse events before hospital discharge: death, MI, recurrent symptoms requiring urgent repeat target vessel revascularisation (TVR) with PCI or coronary artery bypass graft (CABG) surgery, tamponade requiring pericardiocentesis or surgery, and stroke. Long-term MACE was defined as all-cause mortality, stroke, MI and TVR.
All patients underwent follow-up by the CTO team. All MACE were prospectively recorded. Outcomes are reported at the longest follow-up time available.
No local research ethical committee approval or NHS research permissions were required for this study as it was a retrospective analysis of a de-identified administrative database and the project/findings represent service evaluation.
All authors had full access to all of the data in the study and take full responsibility for its integrity and data analysis.
Statistical Analysis
Continuous variables are expressed as mean ± SD. Categorical variables are expressed as a percentage.
Results
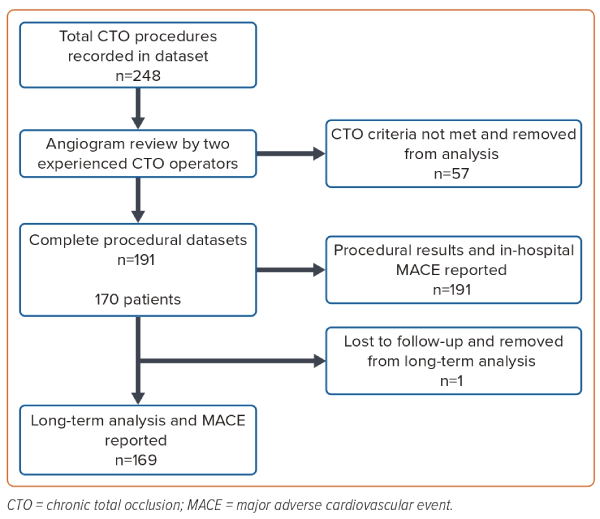
A total of 248 CTO procedures were recorded in the PCI database during the study period. Following detailed review of the angiograms and clinical data, 57 patients were excluded from further analysis as CTO diagnostic criteria were not met. The main reasons for the exclusion of these cases were recent coronary occlusion (<3 months) based on a clear history of recent acute coronary syndrome/symptoms or the presence of a functionally occluded vessel on coronary angiography with antegrade TIMI 1–2 flow in the distal vessel. These cases had erroneously been classified as and entered on the PCI database as CTOs. One patient who was from outside the area was lost to follow-up and removed from long-term data analysis. We therefore report on the acute outcome of 191 CTO procedures in 170 patients with long-term outcomes in 169 patients (99.4%; Figure 1).
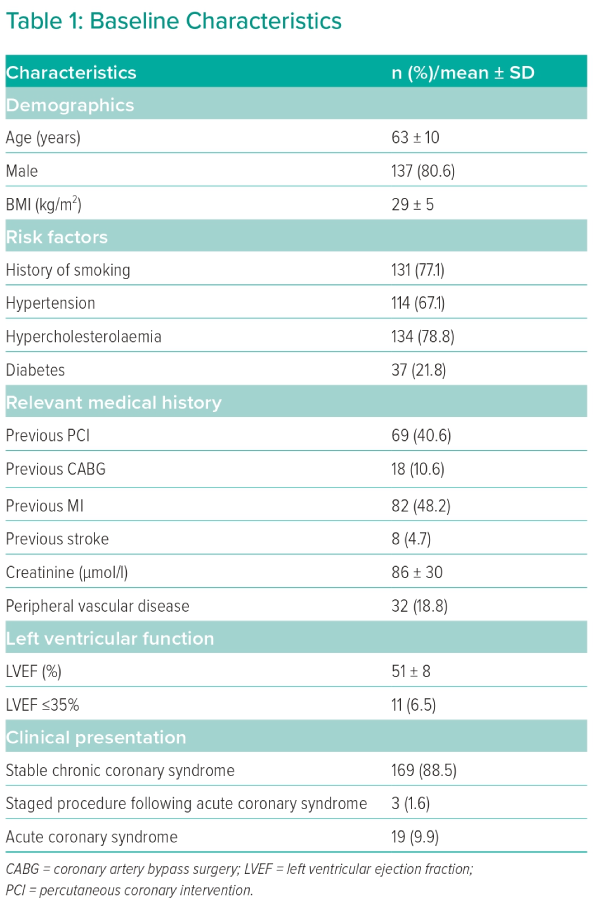
Baseline demographics are presented in Table 1. The mean age was 63 ± 10 years and 80.6% of patients were men. In total, 21.8% had diabetes, 10.6% had prior CABG surgery, 48.2% had a previous MI and 18.8% had a history of peripheral vascular disease. The vast majority (88.5%) of procedures were performed electively in patients with stable chronic coronary disease.
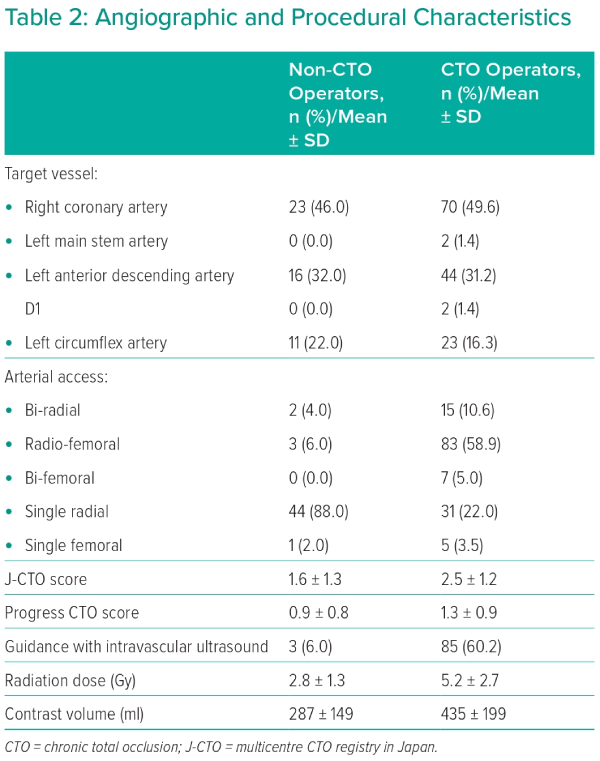
Procedural characteristics are outlined in Table 2. CTO lesions were complex with an overall mean J-CTO score of 2.3 ± 1.3 and Progress CTO score of 1.2 ± 0.9. The right coronary artery was the most common target vessel for intervention, accounting for 48.6% (n=93) of total procedures. Dual-catheter access was used in 74.4% of cases when the procedure was performed by the CTO team. The rate of intravascular imaging with intravascular ultrasound (IVUS) following successful lesion crossing was higher when the procedure was undertaken by a dedicated CTO operator (60.3%; n=85), compared to a general interventionalist (6.0%; n=3). During the study period, the rate of IVUS use increased from 53.8% in 2015 to 76.5% in 2019.
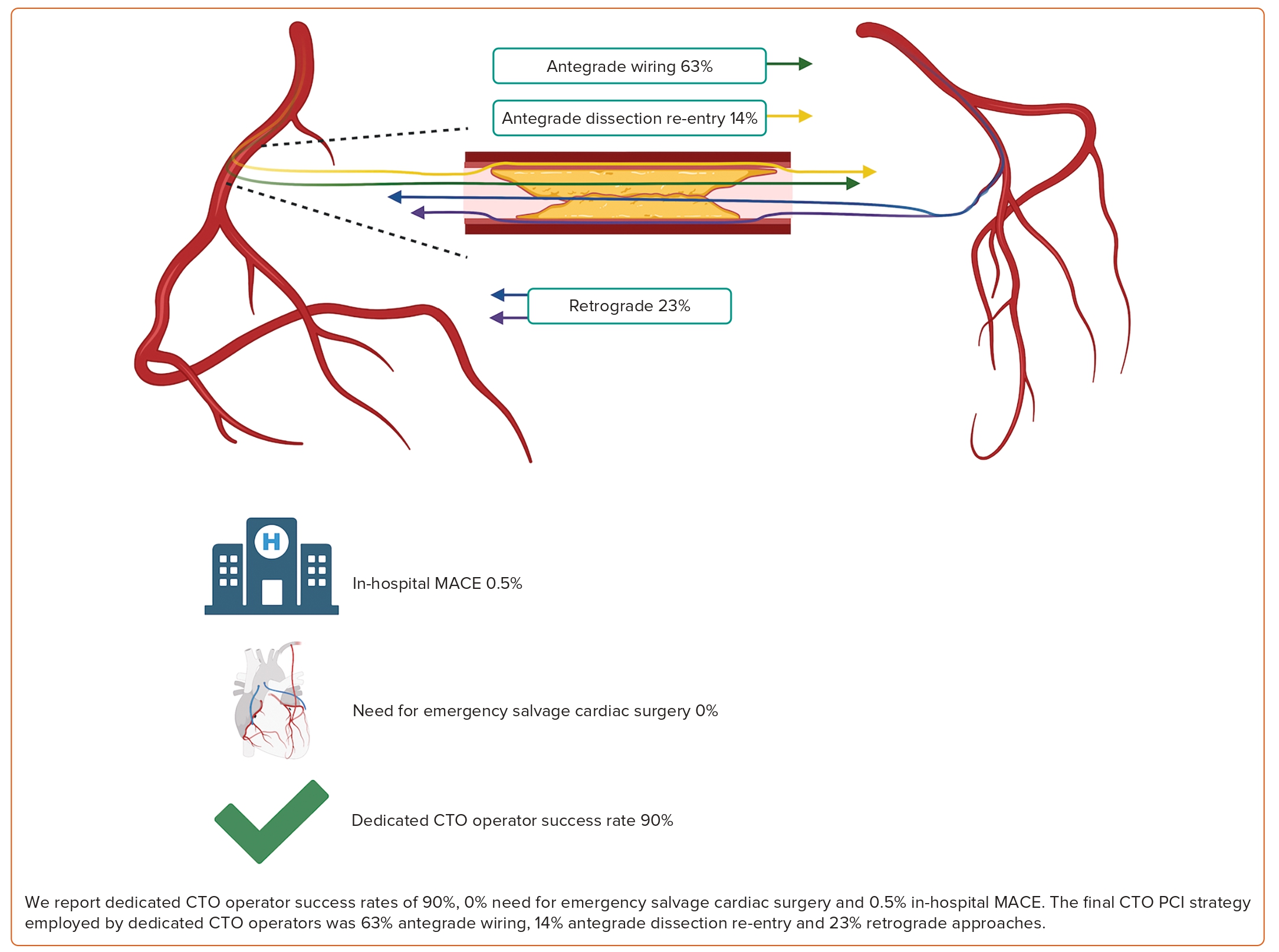
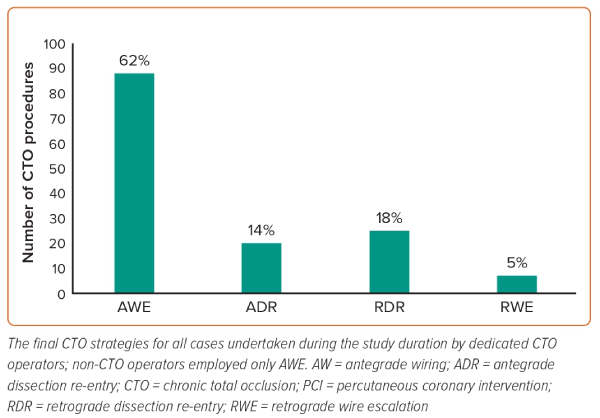
Procedural strategies are outlined in Figure 2. All CTO PCI by the non-CTO operators was with antegrade wiring. The final PCI strategies used by CTO operators were: antegrade wiring in 88 of 141 patients (62.4%); antegrade dissection and re-entry in 20 of 141 patients (14.2%); retrograde wire escalation in seven of 141 patients (5.0%); and retrograde dissection and re-entry in 26 of 141 patients (18.4%). All patients were treated with dual antiplatelet therapy and guideline-directed secondary prevention treatment.
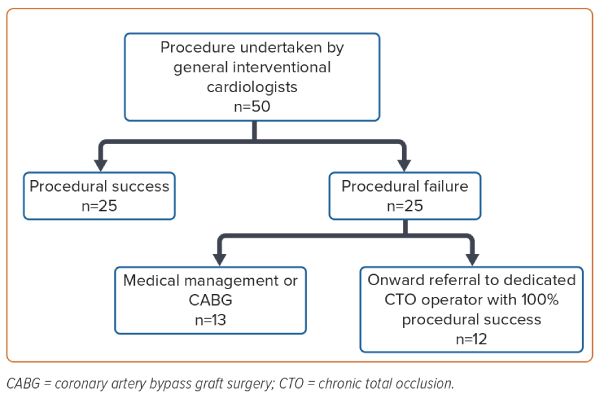
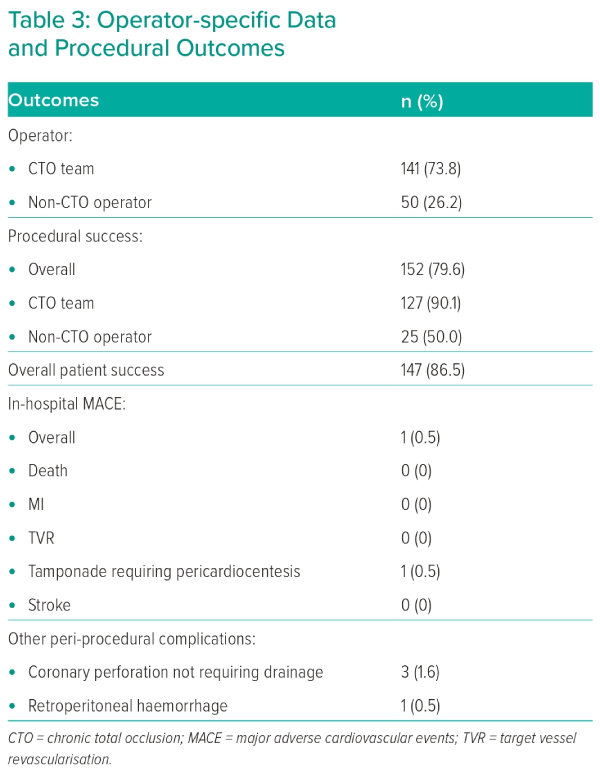
A total of 50 CTO PCI procedures were undertaken by non-CTO operators with a procedural success rate of 50.0%. Of the 25 patients who had an initial unsuccessful attempt at CTO PCI by non-CTO operators, 12 were referred onward to a dedicated CTO operator for coronary intervention. All 12 patients subsequently underwent successful CTO PCI by the CTO team (Figure 3). The remaining patients were either referred for CABG surgery or managed medically. The most common reason for procedural failure by general interventional cardiologist was inability to successfully cross the CTO with a wire (56.0%; n=14) or extraplaque wire position.
Of the 141 procedures undertaken by dedicated CTO operators, procedural success was achieved in 127 CTOs (90.1%). Only 14 procedural failures at the index procedure were reported, of which 21.4% (n=3) were due to failure to cross the lesion with a coronary wire and >50% residual coronary stenosis in 21.4% (n=3). Four patients within this group were brought back for a second attempt at CTO PCI, 100% of which were successful. Thirteen patients underwent modification of the subintimal space as an investment procedure. The subsequent CTO attempts were successful in seven (53.8%) of these patients.
The overall procedural complication rate was low. In-hospital MACE occurred in only one patient (0.5%), who developed cardiac tamponade requiring pericardiocentesis. There was no incidence of stroke and no reported cases of radiation dermatitis. There were no instances of peri-procedural acute kidney injury requiring dialysis. Other non-MACE complications occurred in four patients (2.1%): three coronary perforations that were managed conservatively and one patient who developed retroperitoneal haemorrhage (Table 3). During the study period, no salvage or emergency rescue CABG surgery was required for any patients undergoing attempted CTO PCI in our centre.
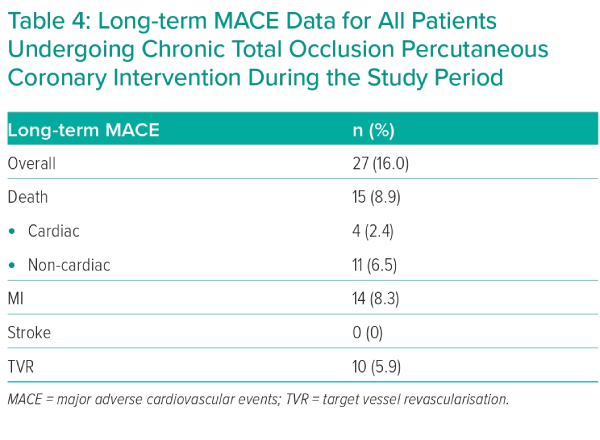
Long-term MACE data were available for 169 patients with a median follow-up of 3.8 years (interquartile range 2.4–5.0) and a maximum follow-up of 6.4 years (Table 4). There were four cardiac deaths. A total of 11 patients had a non-cardiac death, six of which were due to malignancy. During the follow-up period, 14 spontaneous MIs occurred, and 10 TVR procedures were undertaken, five of which necessitated CABG surgery. There was no incidence of stent thrombosis.
Discussion
The primary objective of this retrospective cohort study was to evaluate the feasibility, safety and success of CTO PCI in a high-volume PCI centre without on-site surgical support. The main findings of this study are: high procedural success (90.1%) with low complication rates is achievable when the intervention is undertaken by dedicated CTO operators; long-term MACE rates are low when the intervention is carried out by experienced hands; and patients who have onward referral to dedicated CTO operators after a failed initial attempt have excellent outcomes.
This is the first large-scale report of the feasibility, safety and long-term outcome of CTO PCI in a NSC. The only other report of CTO PCI with remote surgical back-up is a small retrospective study in 18 selected patients in whom CTO PCI was attempted using only the antegrade intraluminal wiring technique.22 To the best of our knowledge, our study is the first report of CTO PCI in an NSC, in all comers, using all modalities of the hybrid algorithm. Overall, our findings suggest that CTO PCI without on-site surgical cover is both safe and effective when undertaken by experienced operators trained in hybrid approaches.
Historically, PCI was undertaken only in centres with on-site cardiothoracic surgical back-up. The increasing move towards PCI being performed without on-site surgical support initially met resistance but it is now commonly practised, with similar outcomes to those carried out in surgical centres.23 Currently, in the UK, almost half of all PCI procedures are undertaken in NSCs, although this is much lower for CTO PCI.5 Furthermore, the incidence of transfer for emergency CABG following PCI in the UK has fallen dramatically over the last two decades from 2.6% to 0.05% of all procedures.24
We have recently reported on the safety and feasibility of high-risk left main (LM) PCI in our NSC.25 A recent retrospective analysis of the BCIS LM PCI procedures has reported similar findings with no evidence of increased mortality, in-hospital MACE or emergency CABG surgery in NSCs, despite higher disease complexity.26 Based on our favourable experience with high-risk PCI in our NSC, along with evolving technology, experience and safety of CTO PCI, we have set up a dedicated CTO PCI programme in our unit.27
Coronary CTOs remain the most challenging lesions to treat with PCI and have a considerably higher rate of procedural complications than elective non-CTO PCI.28,29 Accordingly, there have been suggestions that CTO PCI should be performed only at hospitals with on-site surgery facilities.18 There are no formal criteria in the UK regarding which patients can or cannot be treated at NSCs provided that the appropriate expertise and equipment is available.24,30 Similarly, in the global expert consensus document for CTO PCI, there are no specific recommendations suggesting surgical back-up is needed, although it is highlighted that outcomes are less optimal at less experienced centres.31
The findings from our study attest to the feasibility, safety and efficacy of such a programme when PCI is performed by experienced operators. Our procedural success rate of 90.1% when PCI was undertaken by the CTO team is comparable to that of contemporary large-scale registry data.32 Our in-hospital MACE rate of 0.5% was much lower than that reported in older large-scale registries. The European Registry of Chronic Total Occlusion and the OPEN-CTO registry reported in-hospital MACE rates of 4.4–5.2% and 7.0%, respectively.33,34 The historic Japanese J-CTO registry also reported similar figures.35 More contemporary registry data from China report lower 30-day MACE rates of 0.9–1.5%, likely reflecting improvements in CTO PCI technology and operator experience and skill.27 These results have been reflected in recent Japanese, German, Canadian and Dutch registry data.13,15,17,36
The extremely low in-hospital MACE rate in our study is likely to be related to underestimation of the rate of peri-procedural MI, resulting from the lack of systematic measurement of cardiac biomarkers. This practice relates to the high rate of same-day discharge of our elective uncomplicated CTO PCI patients. Moreover, there have been variability and uncertainty regarding the definition and clinical significance of peri-procedural elevations in cardiac biomarkers. In a recent large cohort of patients undergoing CTO PCI by an experienced group of Chinese high-volume CTO operators, the long-term risk of cardiovascular death was predicted by a creatine kinase myocardial band (CKMB) ≥5 times the upper reference limit but not by an elevated peak troponin I.37 We do not routinely measure CKMB in our unit.
CTOs remain the most difficult lesions to treat percutaneously. These technical challenges –along with operator discomfort, historically low success rates and misconceptions regarding the absence of ischaemia in non-infarcted myocardium supplied by a CTO due to the presence of collaterals and the ongoing debate about the impact of elective CTO PCI on survival – have resulted in the presence of a CTO being a significant predictor of incomplete revascularisation.4,29
These same factors possibly contribute to a reluctance to refer patients with a CTO to a dedicated CTO team resulting in undertreatment of this coronary lesion subset when clinically indicated.
However, due to both technological advances and adoption of algorithm-based approaches to CTO recanalisation, the success of CTO PCI has significantly improved in the past decade, with a progressive reduction in procedural complications.
Based on the high technical success rate achieved by the CTO team in our study, along with the low rate of in-hospital complications, we would argue that it is entirely safe and effective to perform CTO PCI in NSCs. None of the patients in our cohort needed transfer to the regional centre for emergency CABG surgery. This finding is comparable to that from the CONSISTENT, OPEN-CTO and RECHARGE registries and the Euro CTO trial.11,20,34,38 Perhaps more important than having cardiothoracic surgical back-up on site is ensuring that the whole team are fully trained/proctored in all aspects of CTO PCI, including having the expertise to perform all strategies required by the hybrid algorithm, as well as having familiarity with and the skillset to use the dedicated equipment needed to deal with any potential procedural complications.
Limitations
Our study has several strengths including its modest size and near completeness of long-term follow-up. Furthermore, this is a real-world description of the success of a dedicated CTO programme in a large NSC. However, it has a number of limitations. First, it represents a single NSC’s experience of CTO PCI performed predominantly by an experienced team trained in hybrid approaches. Our findings may therefore not be generalisable to all NSCs.
Second, all demographic, procedural and outcome data were collected retrospectively from medical notes and electronic patient records, and we cannot completely rule out bias in the reporting of post-procedural events.
Third, pre- and post-procedural angiograms and procedural outcomes have been reported by the respective operators and not adjudicated by a core laboratory.
Fourth – and perhaps the main limitation of our study – is that we did not systematically measure pre- and post-procedural cardiac biomarkers in all our patients, with measurements performed only if clinically indicated as per our routine practice. This will certainly have resulted in an underestimation of peri-procedural MI.
Conclusion
Our results suggest that CTO PCI without on-site surgical cover is both safe and effective when procedures are undertaken by experienced high-volume teams with the skillset to perform all modalities of the hybrid algorithm, with good in-hospital and long-term outcomes.
We anticipate that the results from our study may have an impact on the provision of CTO PCI in NSCs, traditionally only undertaken in centres with on-site surgical back-up. 
Clinical Perspective
- Chronic total occlusion (CTO) percutaneous coronary intervention (PCI) success and complication rates have significantly improved over the past decade.
- However, the risks involved remain higher than those for non-CTO PCI and the procedure should be undertaken only by experienced teams.
- Because of its less favourable benefit:risk ratio, CTO PCI has traditionally been undertaken only in centres with on-site cardiothoracic surgical back-up.
- This is the first large-scale report of CTO PCI outcomes in a centre with no on-site cardiac surgical facilities.
- The results indicate high technical success and low in-hospital complication rates, attesting to the feasibility, safety and favourable outcome of CTO PCI in an experienced non-surgical centre.
- We anticipate that our results may have an impact on the proportion of CTO PCI undertaken outside surgical centres.