Percutaneous coronary intervention (PCI) in heavily calcified coronary stenoses is particularly complex. Lesion preparation is critical, and various plaque modification techniques are available. The PREPARE-CALC (Comparison of Strategies to Prepare Severely Calcified Coronary Lesions) trial demonstrated superior strategy success for calcified lesion preparation with rotational atherectomy (RA) over modified balloon (MB) techniques.1
Female sex has been linked to a poorer prognosis after coronary revascularisation. A higher risk of death, MI and complications in women undergoing PCI has been demonstrated in various studies, presumably due to older age, a higher prevalence of comorbidities, and a more severe coronary artery disease (CAD) risk profile at the time of presentation.2–7
The combination of female sex and heavily calcified lesions appears to be particularly synergistic. Although women tend to present less frequently with severely calcified coronary lesions, significant sex differences to the detriment of women have been found in terms of complications such as death, MI, stent thrombosis, stroke and target lesion revascularisation.1,8
It has been previously suggested that women, due to sex-specific peculiarities in arterial access, bleeding risk and coronary pathophysiology, may be particularly susceptible to complications (especially coronary artery perforation) following RA compared with men.9–11
In the context of this setting, the aim of this study, a sub-analysis of the PREPARE-CALC trial, was to investigate the sex-specific differences in calcified coronaries in general and according to different lesion preparation strategies.
Methods
Patients and Study Design
Design details including inclusion and exclusion criteria of the open-label, multicentre, randomised PREPARE-CALC trial have been published previously.1 In brief, patients undergoing PCI with severely calcified coronary lesions were randomised 1:1 to either RA or MB treatment, followed by implantation of a new-generation sirolimus-eluting stent.1 Importantly, patients with MI ≤1 week prior to the procedure and patients with target vessel thrombus were excluded from PREPARE-CALC. All patients gave written informed consent. The study was conducted in accordance with the provisions of the Declaration of Helsinki and with the International Conference on Harmonisation Good Clinical Practice guidelines.12 The trial protocol was approved by the institutional ethics committee of the two participating centres.
Endpoints
In line with the main trial, the primary endpoints of the current analysis were strategy success and in-stent late lumen loss (LLL) at 9 months in women and men. Strategy success was defined as successful stent delivery and expansion with attainment of <20% in-stent residual stenosis of the target lesion in the presence of Thrombolysis in MI (TIMI) 3 flow without crossing over or stent failure. In-stent LLL was defined as the difference between the post-procedure and 9-month in-stent angiographic minimal lumen diameter. If the strategy failed, the underlying cause was determined. As secondary outcomes, adverse events during hospitalisation, specifically death, MI, target-vessel re-PCI, bypass operation, stent thrombosis, and coronary perforation were also assessed.
Additional analyses included comparison of baseline, procedural and angiographic characteristics as well as findings from intracoronary imaging according to sex.
Optical Coherence Tomography Subgroup Analysis
For the intracoronary imaging analysis, we analysed optical coherence tomography (OCT) data, when available, in order to elicit possible explanations for differences between the treatment groups at the level of vessel architecture. Image acquisition was performed with the ILUMIEN OPTIS console and the Dragonfly intravascular imaging catheter (St Jude Medical). Matched OCT data (pre- and post-procedure) had originally been assessed by a core lab. Specific parameters designed to assess the burden of calcification, including maximum calcium arc, average calcium arc, maximum plaque thickness, mean cap thickness, total volume of calcified plaque, total length of calcified plaque, indexed volume of calcified plaque and OCT-based calcium score were compared. Definitions are as previously outlined.13
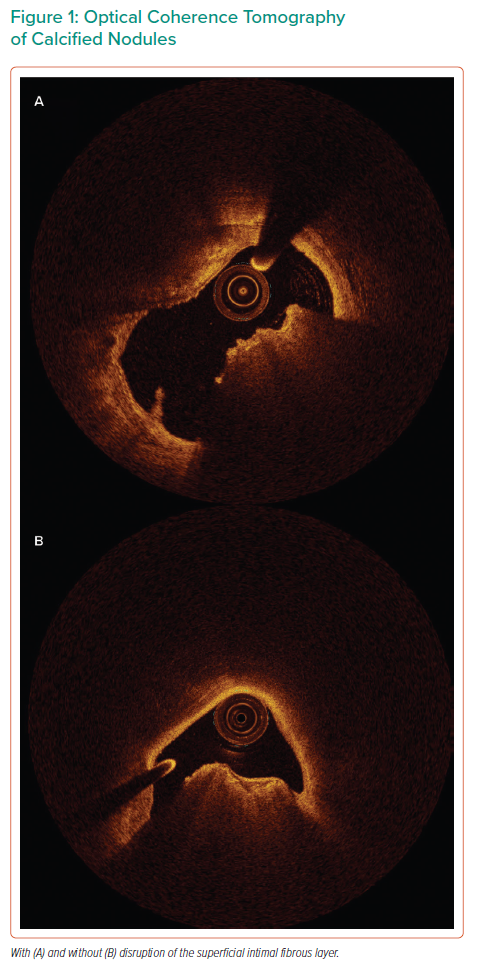
We extended the analysis to include a more detailed assessment of the characteristics of calcified nodules than had been undertaken at the core lab. We defined a calcified nodule as an intraluminal protrusion of nodular calcification.14 Specifically, we used this OCT-based definition, rather than the pathological definition of a calcified nodule, given that we are performing an OCT and not a pathological examination to assess their presence or absence. We distinguished between the presence and absence of disruption of the fibrotic cap of calcified nodules (Figure 1), and we recorded the lumen area at the site of the calcific nodule, its base dimension and height, and the number of calcified nodules per case.
Statistical Analysis
Analysis was by intention to treat. Continuous data are presented as mean ± SD, or median and interquartile range, as appropriate. Categorical data are presented as counts and proportions (%). Differences between groups were checked for significance using the Student’s t-test or Mann–Whitney U-test (for continuous data) or the chi-squared or Fisher’s exact test as required. For lesion-level data, differences between groups were checked for significance using generalised estimating equations to address intrapatient correlation in patients who underwent multi-lesion intervention. All tests were two-sided, and a p-value of <0.05 was considered statistically significant. For non-inferiority testing of MB versus RA in terms of 9-month LLL, a non-inferiority margin of 0.2 mm was taken, in line with the main PREPARE-CALC study, and based on LLL data from the earlier randomised ROTAXUS study.1,15 Interaction analyses were performed by including an interaction term in a multivariate regression model derived to predict the variable of interest, either linear or logistic as appropriate, depending on whether the variable was numerical or representative of a binary outcome. The Fisher-Freeman-Halton test was used to make comparisons in contingency tables with more than two possible outcomes. Data analysis was performed using SPSS (version 27.0.0.0, IBM). The steering committee had full access to the data and took responsibility for its integrity and that of the data analysis.
Results
Baseline Characteristics
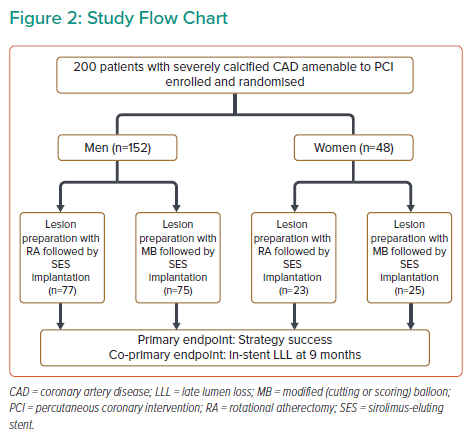
Of the 200 randomised patients, 48 were women (24%) and 152 were men (76%) (Figure 2). Overall, the baseline clinical and angiographic characteristics were similar between men and women (Supplementary Material Tables 1 and 2), with the exception that women were more likely to have impaired baseline renal function while men were more likely to be smokers and have a lower left ventricular ejection fraction. For those patients randomised to RA, no significant difference in burr size between male and female patients was noted (1.5 ± 0.2 mm for women versus 1.5 ± 0.2 mm for men, p=0.39), while for the patients randomised to MB, no difference in the size of MB used was noted (2.90 ± 0.36 mm for women versus 2.98 ± 0.33 mm for men, p=0.26), with these balloons being inflated to similar pressures (16.26 ± 3.84 atm for women versus 15.48 ± 2.80 atm for men, p=0.36; Supplementary Material Table 3).
Clinical Outcomes
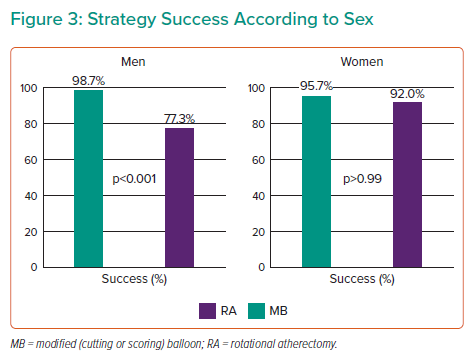
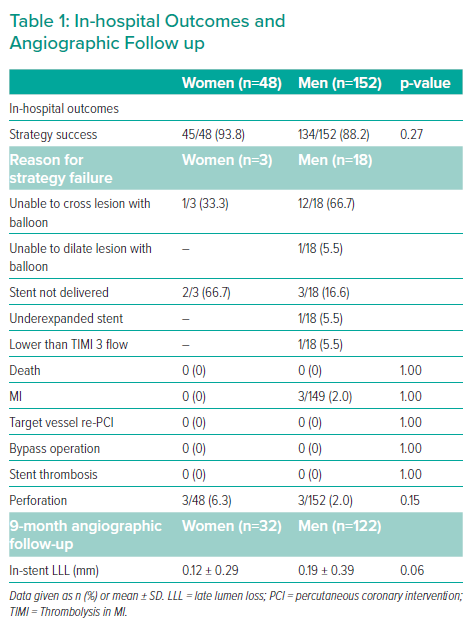
Strategy success was achieved in 88.2% of cases for men and in 93.8% of cases for women (p=0.27; Figure 3). No statistically significant differences between sexes were noted regarding both in-hospital events and in-stent LLL at 9 months (Table 1).
Overall, there were few differences in clinical or angiographic characteristics between women and men according to different treatment strategies (Supplementary Material Tables 4 and 5).
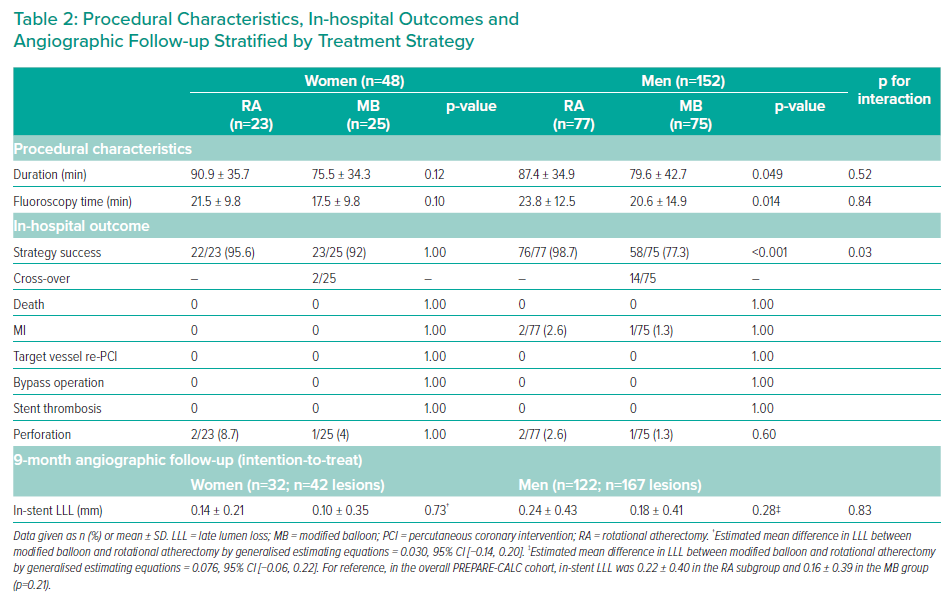
For women, there was no significant difference in strategy success between RA and MB (95.7% in the RA group versus 92% in the MB group, p>0.99). For men, strategy success was significantly more common with an RA-based strategy than an MB-based strategy (98.7% in the RA group versus 77.3% in the MB group, p<0.001) (Table 2 and Figure 3), albeit with significantly longer procedure and fluoroscopy times. For reference, in the overall PREPARE-CALC cohort, strategy success was 98% in the RA group versus 81% in the MB group (p=0.0001). Sex influenced the interaction between strategies and revascularisation success (interaction p=0.03).
Regarding in-hospital events or in-stent LLL at 9 months, no evidence of a difference between women and men according to the lesion preparation strategy was identified. Sex did not influence the interaction between strategies and in-stent LLL at 9 months (interaction p=0.83). A formal test for non-inferiority of MB to RA in the respective subgroups was carried out, but due to the limited numbers in both respective subgroups, non-inferiority could not be established (Table 2).
Of note, although the numbers were small overall, and not statistically significant, the rate of perforations was found to be proportionally higher in women than in men, at 3/152 (2.0%) for men and 3/48 (6.3%) for women. Similarly, in both the women and the men, two perforations occurred in the RA subgroup and one in the MB subgroup.
Optical Coherence Tomography Subgroup Analysis
Those patients who could be included in the OCT subgroup analysis (n=105) are summarised in Supplementary Material Figure 1, and the findings in Supplementary Material Table 6. Supplementary Material Table 7 lists the reasons why OCT was not possible in the remaining cases, the majority being because it was not possible to cross the lesion with the OCT catheter. Plaque rupture before intervention was found to be more frequent in women (21.9%) than in men (4.4%, p=0.007), although the incidence of this finding was low overall, in keeping with the fact that the enrolled patients did not present with acute MI. Parameters that traditionally classify the burden of calcification on OCT were not found to be significantly different between groups (Supplementary Material Table 6). A detailed analysis of calcified nodules (Supplementary Material Tables 8 and 9) found no difference between groups overall (presence in men 78.9% versus 65.6% in women, p=0.14), whereas a significantly higher number of calcified nodules with disruption of the superficial intimal fibrous area was noted in women (57.1%) versus men (28.2%, p=0.014).
Post-stenting OCT showed significant differences in terms of maximum stent eccentricity (men 0.69 ± 0.07 versus women 0.72 ± 0.04, p=0.02), stent eccentricity <0.7 (men 48% versus women 23.3%, p=0.02) and lumen eccentricity index <0.7 (men 77.3% versus women 53.3%, p=0.02). When individual subgroups of men and women were analysed by treatment strategy, there were no OCT features that were found to differ significantly by treatment strategy within the sex subgroups.
Discussion
The present sub-analysis of the PREPARE-CALC trial investigating sex-specific outcomes can be summarised as follows: first, women and men with severely calcified coronary arteries presented with a similar clinical and procedural profile, and due to the randomised nature of PREPARE-CALC, were subject to the same selection (inclusion) criteria, with results from the RA arm being similar in efficacy and safety for both male and female patients. Second, in this specific population, we did not detect a signal suggestive of a difference in overall strategy success between women and men. Third, the mean LLL was similar for both groups across treatment strategies, although the numbers precluded definitive establishment of non-inferiority. Fourth, despite similar clinical and procedural characteristics, the strategy success rates differed for women and men according to the assigned strategy (RA versus MB), with similar results for RA and MB in women, but a significantly more successful RA strategy in men. Finally, although there was no difference between women and men in established measures of calcification on OCT, a significant difference was noted with regard to the number of women versus men with calcified nodules with disruption of the superficial intimal fibrous area and with plaque ruptures, despite the fact that patients with recent MI were excluded from PREPARE-CALC.
Our findings extend previous work in the field of sex differences in coronary interventions. In contrast to prior studies on coronary interventions, in which women presented with a higher risk burden (presumably due to the higher age), in our study women with calcified coronary arteries presented with a similar clinical and procedural profile to men.3,4 Interestingly, the previously reported poorer outcomes for women undergoing RA were not replicated in this study, although the rate of coronary perforation was proportionally higher in women, and numerically higher in the RA subgroups, without reaching statistical significance. This differs from an analysis of 765 consecutive RA procedures in a regional referral centre in Scotland, of which 37% were carried out in female patients, showing that women were more likely to experience complications during RA, specifically coronary dissection, cardiac tamponade and significant bleeding, and thus, that there was a greater incidence of net adverse cardiac events for women than men in the setting of an RA strategy.9 Furthermore, several studies have shown an association between coronary perforation and female sex, with and without RA.16,17 Indeed, in one series female patients accounted for 50% of perforations, despite comprising only 26% of cases overall.16 This difference may be explained by the fact that our study is unique in that it uses data obtained from a randomised controlled trial, which has the advantage of reducing selection bias, although due to the characteristics of the overall population from which the patient sample was drawn, and the fact that only 24% of participants in the trial were women, it is possible that this selection bias is not entirely eliminated by the randomisation process.
Along parallel lines, in the specific setting of a population with a very high baseline calcified plaque burden, with a maximal calcified plaque arc of 267.4° for women and 247.9° for men, a maximum plaque thickness of 1.35 and 1.25 mm, respectively, and a total length of calcification of 23.6 and 22.2 mm, respectively, despite the similarities in baseline clinical characteristics, our data suggested relevant differences in terms of strategy success for women and men according to the assigned strategy. While both strategies appeared to show similar results in women, the RA strategy was significantly more successful in men. Thus, it follows that we observe a larger number of cross-overs in the male MB subgroup, and as a corollary given the sex-specific differences in terms of sample size (with a higher proportion of men than women), this explains the results of the PREPARE-CALC trial, in which RA showed overall superiority.1 Although limited in terms of statistical power by the number of female patients included in the PREPARE-CALC study, as a hypothesis-generating point of discussion, it is nonetheless interesting and merits further evaluation in future clinical studies with a greater number of female patients enrolled.
Furthermore, the lack of detection of a difference in mean LLL across treatment strategies between women and men suggests that there may be a similar long-term response of the arterial wall to stenting overall, regardless of the method of lesion preparation.
OCT analysis showed sex-specific differences with regard to the proportion of patients with plaque rupture and calcified nodules with disruption of the superficial intimal fibrous area at baseline. It is important to emphasise that these findings are not in the setting of an ongoing MI, by means of the exclusion criteria of PREPARE-CALC, but instead are incidental, in keeping with the fact that most atherosclerotic plaques destabilise without resulting in a clinical syndrome, and that this process is particularly common in those patients with chronic manifestations of atherosclerotic disease.18,19 For plaque ruptures, our finding of a greater prevalence in female patients than in male patients differs to that found in historical studies, but interestingly, more recent studies have found, albeit in the ACS setting, that female sex had no significant impact on the proportion of patients with plaque rupture at OCT analysis.20–23 In a separate study this was also found to be the case for plaque erosion, with age rather than sex being the determining factor.24 In the case of calcified nodules, in one previous study no difference was found between the proportions of men and women; however, this was a general population with CAD referred for PCI, rather than those specifically with heavy calcification, and thus the proportion of patients with calcified nodules was much lower than in our study (3.6% for men and 4.6% for women).25 Interestingly, however, although a second study found a similar prevalence of calcified nodules overall, more calcified nodules were noted in women than in men.26 Furthermore, in those patients with lesions with a maximum calcium arc >180°, 30% of ACS culprit lesions contained a calcified nodule. Of note, in that study, the authors excluded lesions with anticipated difficulty in passing the OCT catheter, including angiographic severe calcification. Thus, it may be that the true prevalence of calcified nodules has been underestimated previously, and is in fact much higher in a patient population in whom the majority of lesions have severe calcification. Thus, the proportion of plaque ruptures and calcified nodules may be a reflection of this cohort of female patients with extensive calcific disease, rather than only a reflection of sex.
Only one other study in the literature has been identified in which, using OCT imaging, the difference in calcified plaque parameters between men and women was investigated.27 Women <70 years old who underwent OCT and PCI in a single centre in Japan, the majority for stable CAD, were found to have a significantly higher prevalence of calcification with an arc ≥180° on cross-sectional imaging, but otherwise no differences were noted. In our study, measures of OCT plaque calcium quantification (number of plaques, plaque angle, plaque thickness, cap thickness, maximum and mean total calcium area per frame, true indexed calcium volume) did not differ significantly between male and female patients, however, we did note differences in maximum stent eccentricity and lumen eccentricity index <0.7. It is possible that there is a link between the higher proportion of calcified nodules with disruption of the superficial intimal fibrous area and plaque ruptures in women, and a lower frequency of stent eccentricity after PCI, suggesting that the calcific lesions in women in this study are more easily modified (in particular by MB), but the limitations of our data (in particular, that OCT could not be used in all cases) necessitate further work to clarify this point.
Ultimately, the results of this subgroup analysis might have important clinical consequences in the context of the overall trial in a cohort of patients with extensive stable calcific CAD, suggesting that while women may be more likely to have lesion characteristics amenable to vessel preparation with MB as opposed to requiring RA, a primary RA strategy may be considered for men. Nonetheless, given the disparate findings compared with previous registries, further investigation is warranted, particularly given that detailed analysis of the available OCT data does not show a clear mechanistic cause.
Some limitations merit consideration. First, the number of women included in the present study was lower compared with men, and as a consequence the statistical power is limited. In particular, given the number of women as a proportion of the total number of trial participants (24%), there is a risk that population effects are not detected in this sample due to the limited size. Furthermore, the total number of patients included is relatively modest. Thus, this subgroup analysis leads to findings that may be viewed only as hypothesis-generating rather than definitive. According to previous studies, women are still underrepresented in trials assessing coronary interventions and the rate of enrolled women is still far from 50%.28 The reason for this underrepresentation is still unclear. It might be due to the lower incidence in terms of CAD, which leads to lower inclusion in these trials. Still, all these data seem to suggest that efforts need to be made in order to mitigate the sex misbalance in terms of enrolled patients, for example by stratified randomisation of women. Second, as outlined above, matched OCT data were not available for all cases, only in 105 of 200 patients. Third, the limitations of the original PREPARE-CALC trial also hold, specifically that patients who had had an MI ≤1 week prior to the procedure were excluded, and that although MB refers to either scoring or cutting balloons, in the majority of cases scoring balloons were used. Finally, during the time period in which this trial was carried out, intravascular lithotripsy was not available. Its development and early clinical studies have subsequently added a new device to the armamentarium of the interventional cardiologist and may be particularly useful in those cases in which it is possible to cross the lesion with a balloon, but in which the balloon cannot be fully dilated or a stent cannot be delivered.29–31 Although direct head-to-head comparisons with MB and RA are still required, this may temper our approach to calcium modification.
Conclusion
Although women with calcified coronary arteries presented with a similar clinical and procedural profile to men, in terms of strategy success the RA strategy was superior in men whereas in women both the RA and MB strategies appeared to have a similar success rate. These data suggest that for women both the RA and MB strategies seem safe and efficient.
Click here to view Supplementary Material.
Clinical Perspective
- Patients with complex calcified coronary artery disease represent a particularly challenging subset of patients to treat percutaneously. Although prior studies have shown sex-based differences to the detriment of women, these were not replicated in the current study.
- Although RA and MB may not lead to differing strategy success for women, this is not the case for men, with RA in men being more successful.
- This may have important implications for the choice of initial lesion preparation strategy in male versus female patients, although further work is required to clarify why it is the case.