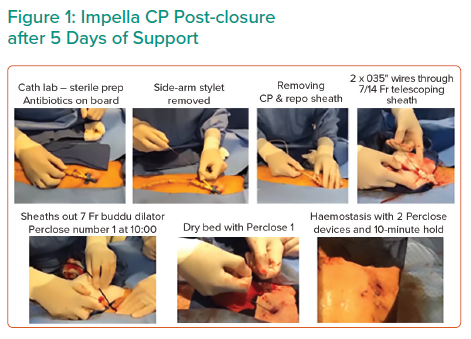
Dr George began his talk by introducing the ST-segment elevation MI (STEMI)-Door-to-Unload (DTU) pilot trial. The 3-year study investigated whether left ventricular (LV) mechanical unloading with an Impella CP transvalvular pump for 30 minutes prior to reperfusion in STEMI patients as a potential means to limit infarct scar size was safe and feasible.1 Fifty anterior STEMI patients received an Impella CP device to assess safety and feasibility during a heart attack. The patients were randomised to receive ventricular unloading with immediate percutaneous coronary intervention (PCI) or ventricular unloading for 30 minutes prior to reperfusion. An MRI before and after the process was used to determine infarct size. The Impella device was removed after a minimum of 3 hours of support. Dr George commented that the use of the post-closure technique, shown in Figure 1, has been shown to improve clinical outcomes.2
The STEMI-DTU pilot trial results confirmed the safety and feasibility of STEMI trial randomisation, and demonstrated that unloading with delayed reperfusion by 30 minutes limits infarct size, irrespective of the MI area at risk. Mechanical unloading reduces myocardial ischaemia prior to PCI, with increased exposure time to unloading prior to PCI time decreasing infract size in STEMI-DTU pilot trial patients with large anterior MI.3 These results enabled initiation of the currently enrolling STEMI-DTU pivotal randomised clinical trial to confirm whether LV unloading limits infarct size and reduces heart failure after STEMI in a larger patient sample.
Dr George summarised the case of one of the 10 patients enrolled in the STEMI-DTU pivotal trial. A 57-year-old man with previous tobacco use, hyperlipidaemia and blood pressure issues experienced stuttering chest pain for several days. He presented with an abrupt onset of chest pain 30 minutes prior to arrival in the emergency room. ECGs transmitted in the ambulance identified STEMI. The patient met enrolment criteria with willingness to obtain an MRI, non-shock status, blood pressure values in the 130s, heart rate at approximately 110, normal point of care lactate level and dramatic ST-elevation, as determined by ECG.
The patient was randomised to the Impella treatment arm. Upon arrival in the catheterisation lab, fluoroscopic identification of the femoral head using ultrasound and a micropuncture kit enabled meticulous large bore access of the femoral artery. A left ventriculogram enabled placement of the Impella CP. Dr George noted that the additional 20–30 seconds taken to identify appropriate anatomic landmarks during vascular access can minimise complications in trial patients. Immediate unloading with the Impella CP resolved ST-segment elevation in the patient, as detected by ECG, and the patient stated he was pain free upon initiation of the device prior to reperfusion. These observations correlate with prior anecdotal evidence of chest pain resolution and decreased ST-segment with mechanical unloading alone. After unloading, Dr George placed an angioplasty balloon in the patient using the same femoral artery access point. This single-access approach involved micropuncture adjacent to the Impella catheter, inserting an 0.035" wire through the micropuncture, inserting a 6 Fr sheath through the Impella repositioning sheath and then inserting the balloon. Optical coherence tomography (OCT) to identify distal and proximal reference vessel size was performed. Use of the single-access technique instead of two access points by radial technique can decrease vascular complications. After 30 minutes of unloading, Dr George performed PCI, followed by OCT. Placement of an Xience 3.5 × 23.0 mm drug-eluting stent appeared to be angiographically adequate, but OCT imaging indicated poor opposition in the proximal segment of the blood vessel. Such a configuration could produce acute stent thrombosis. Dr George resolved the issue by consecutive post-dilatation using a 4.0 × 8.0 mm balloon and a 5.0 × 8.0 mm balloon.
The final post-PCI angiogram revealed excellent results for the patient with normal distal flow, no residual stenosis and no additional complications. Removal of the catheter sheath produced no bleeding. Post-PCI ECG indicated that ST-segments continued to be resolved. An echocardiogram on days 1 and 30 post-MI revealed resolution of a pronounced wall motion abnormality and LV function restoration. An MRI on days 3 and 30 post-Impella also revealed resolution of the wall motion abnormality, as well as resolution of anterior oedema and hypokinesis.
Dr George concluded that the patient provided an excellent example of trial enrolment, MI resolution immediately after unloading, single-access technique and post-closure technique. Meticulous care of vascular access should be performed from the arteriotomy to post-closure to enable clinical detection of the effect of unloading on infarct size.