Dr Burkhoff opened the meeting by providing an overview of the Acute Cardiac Unloading and REcovery (A-CURE) symposium. The mission of the A-CURE group is to advance the science and mechanistic understanding of acute cardiac unloading and support, and the translation of basic and clinical research into therapies aimed at heart muscle recovery. He noted that the A-CURE symposium is the only scientific conference dedicated entirely to acute unloading and heart recovery.
He described the history of the A-CURE symposium, which began in 2015 with a group of interested investigators in Paris, France. The first annual symposium occurred in 2016 in Rome, Italy, with Dr Eugene Braunwald as the keynote speaker. The commencement of the ST-elevation MI Door-to-Unload (STEMI-DTU) pilot trial was announced in 2017 at the second A-CURE symposium held in Barcelona, Spain, with Dr Valentin Fuster as the keynote speaker. Results of the STEMI-DTU trial were released as a late-breaking abstract at the American Heart Association annual meeting in 2018. The third A-CURE symposium was held in Chicago, Illinois in 2018, with Dr James Udelson as the keynote speaker. The commencement of the STEMI-DTU pivotal trial and PROTECT kidney trial was announced in 2019 at the 4th symposium held in Paris, France, with Dr Douglas Mann as the keynote speaker. This year’s symposium was virtual due to coronavirus disease 2019 (COVID-19) and the associated travel restrictions, and featured a competition for three US$20,000–US$25,000 research grants awarded to the best submitted abstracts, as judged by the A-CURE faculty. In addition, as a response to the global COVID-19 pandemic, Dr Burkhoff announced that A-CURE has developed cardiac-specific educational resources relevant to COVID-19, which are available on the website.
Dr Burkhoff defined ventricular unloading as the reduction of total mechanical power expenditure of the ventricle, which correlates with reductions in myocardial oxygen consumption and the haemodynamic forces that lead to ventricular remodeling.
This year’s symposium focused on cardiac unloading can act as an enabler for other kinds of therapies. Specifically, unloading the heart and assuming its role to support the circulation provides haemodynamic stability, and may enable the application of additional therapies aimed at further protecting the heart or other end-organs. which may otherwise not be possible.
Dr Burkhoff provided examples of such potential future therapies. He described how an implanted unloading device, such as Impella, can provide the cardiac output necessary to support adequate perfusion of end-organs. In the case of acute MI (AMI) complicated by cardiogenic shock, high-dose beta-blockers or ivabradine can be used to slow heart rate and further spare myocardial energetics beyond what may be achievable by unloading alone. The presence of haemodynamic support would minimise the risk for haemodynamic collapse that may result from the use of such drugs during AMI. Similarly, haemodynamic support could be deployed in the setting of therapeutic hypothermia, enabling more rapid cooling of a patient while simultaneously minimising the risk of hypothermia-dependent arrythmia and haemodynamic collapse. In addition, unloading the heart and enhancing end-organ perfusion may be a means of treating cardiorenal syndrome and diuretic resistance in acute decompensated heart failure. Finally, long-term unloading support may also promote reverse remodelling and enhance recovery in patients who otherwise may receive permanent left ventricular assist devices or a heart transplant.
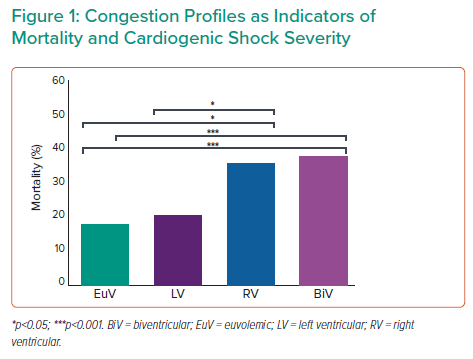
Another goal of this symposium is to advance the current understanding of the role of right ventricular unloading in various clinical settings. Consistent with prior studies, mortality increases markedly in cardiogenic shock patients once central venous pressure or right atrial pressure increases, whether in isolation or in combination with elevations to pulmonary capillary wedge pressure (Figure 1).2 Dr Burkhoff stated that such correlations are also true in patients presenting with acute MI shock and those with acute decompensated heart failure-related shock. Prior A-CURE symposia primarily focused on left ventricular unloading, but a large part of future efforts is to better understand the indications, timing and role of right ventricular support in such patients.
Dr Burkhoff concluded by encouraging virtual attendance at this year’s nine symposium talks and six additional talks selected from the submitted abstracts, as well as in-person attendance at the 6th Annual A-CURE symposium next year.