Osteogenesis imperfecta (OI) is a hereditary defect in collagen type 1 synthesis. Clinical features of OI include blue sclera, hearing loss and pathologic bone fractures.1,2 While uncommon, those affected by OI are at increased risk of cardiovascular abnormalities, particularly left-sided valvulopathies.1,3 In the largest cohort study of OI patients to date, the prevalence of mitral regurgitation (MR) and aortic regurgitation (AR) was estimated at 1.6% and 0.9%, respectively, with an increased cumulative incidence after reaching 50–60 years of age.3 However, surgical intervention on these lesions is hindered by considerable mortality burden and the susceptibility to bleeding and dehiscence of implanted valves.1,2,4 With the emergence of less invasive transcatheter valvular therapies, there remains a limited understanding of the feasibility and durability of these approaches in those with OI and whether they can offer a suitable alternative to conventional surgery. In this context, and with a focus on mitral repair, we report the third case in the literature of mitral transcatheter edge-to-edge repair (MTEER) in a patient with OI and conduct a comprehensive review of the characteristics and outcomes of reported OI cases who underwent surgical or transcatheter mitral repair.
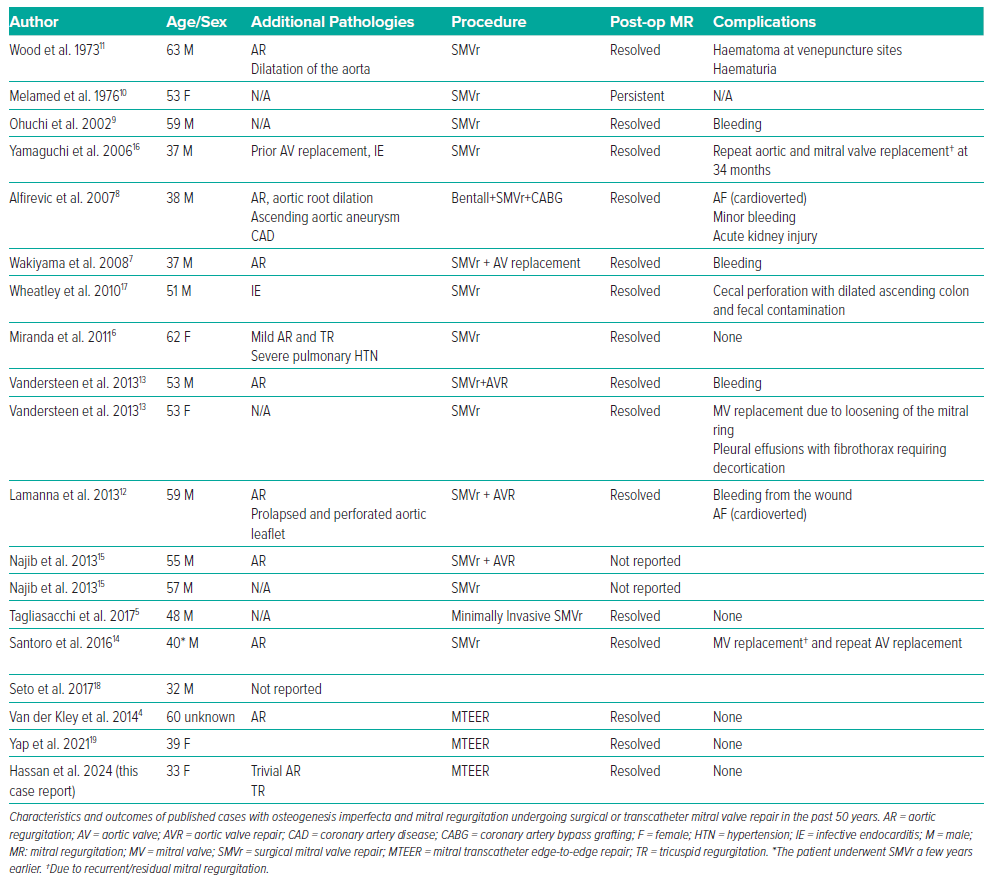
Published cases with OI and MR undergoing surgical or transcatheter mitral valve repair up to date (July 2023) were identified by searching PubMed and Google Scholar using the search terms “osteogenesis imperfecta,” “MitraClip”, “Mitral valve repair”, “mitral repair” and “transcatheter mitral repair”. Two cases of MTEER and 16 cases of surgical mitral valve repair (SMVr) were identified and included in this report (Table 1).4–19
Case Presentation:
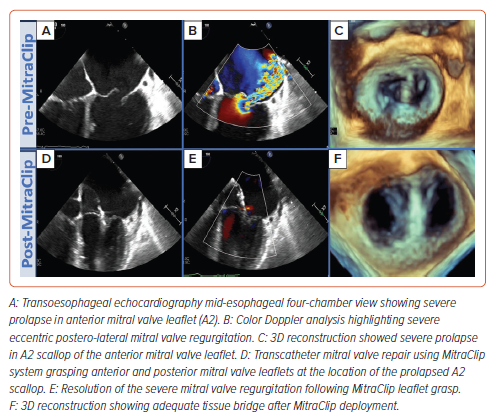
A 33-year-old woman with a history of OI presented to an external medical facility with progressive dyspnoea on minimal exertion and was diagnosed with acute heart failure in the setting of severe MR, she was given diuresis treatment and discharged home. Two months later, she presented again with dyspnoea, which prompted a transfer to the authors’ centre for specialist care. On examination, the patient had ascites, blue sclera, scoliosis, hearing impairment and short stature. Cardiac examination was significant for a grade 5–6 pan-systolic murmur and inspiratory crackles in the lower lung fields. A transoesophageal echocardiogram showed biventricular and biatrial dilatation with preserved left ventricular systolic function, severe eccentric posteriorly directed MR (+4, regurgitant orifice area = 1.8 cm2) caused by mitral valve prolapse of the anterior leaflet at A2 scallop (Figure 1A–C and Supplementary Videos 1 and 2), mild AR, moderate tricuspid valve regurgitation and a right ventricular systolic pressure of 89 mmHg.
Due to the substantial risks associated with open surgery, a percutaneous mitral valve repair was planned. The procedure was conducted via right femoral venous access under fluoroscopic guidance. The MitraClip (Abbott) steerable guide was advanced through the interatrial septum into the left atrium and positioned perpendicular to the coaptation line. After echocardiographic confirmation that the MitraClip was at the site of the prolapsed A2 scallop, the delivery catheter was advanced into the left ventricle. The delivery catheter was slightly retracted to engage the MitraClip device with the targeted scallop and an XTW sized clip was inserted at the A2-P2 segment. Transoesophageal echocardiography confirmed the reduction of MR from severe to trivial with a mean gradient of 4 mmHg (Figure 1C–E; Supplementary Videos 3 and 4). The patient’s post-procedural recovery was uneventful and she was discharged home on the fourth post-procedural day on guideline-directed medical therapy (GDMT). At her 1-month follow-up appointment, the patient was haemodynamically stable and GDMT was well-tolerated. No adverse events or hospitalisations for heart failure were reported at 3-month follow-up.
Discussion
Osteogenesis imperfecta is an autosomally inherited defect in the synthesis of type I collagen, primarily caused by pathogenic variants of COL1A1 and COL1A2 genes.20 In 1965, the first report of cardiovascular manifestations in patients with OI was published, reporting two cases of aortic insufficiency and one case with mitral, aortic and pulmonic valve disease.21 Cardiac surgical intervention in patients with OI constitutes a major clinical challenge. The defective interaction between platelets, endothelial cells, capillaries and abnormal collagen contributes to vascular fragility and high vulnerability to valve dehiscence and cardiac rupture.12,22
In a study of 49 OI patients undergoing cardiac surgery, more than 40% of the cases had postoperative bleeding, and almost 1 in 5 died postoperatively.12
Few cases of SMVr in patients with OI have been reported (n=16; Table 1).5–18 Upon review of these cases, the mean age was 49.8 years ±9.6, with a male-to-female predominance (5:1). A minimally invasive surgical approach was used in one case.5 Echocardiographic features and outcomes were detailed in 13 of these cases.5–13,16–18 A concomitant aortic valve pathology was reported in 69.2% (n=9) of the cases. MR resolution was observed in 92.3% (n=12) of cases, although 46.2% (n=6) and 15.4% (n=2) encountered postoperative bleeding and AF, respectively.5–12 On follow-up evaluation, three cases required MV replacement.13,14,16
Data on the feasibility and durability of transcatheter interventions in this population remain scarce, with only two other cases of MTEER reported in OI patients.4,19 Van der Kley et al. detailed a case of a 60-year-old patient undergoing MTEER with an uneventful postoperative course. This was done under fluoroscopy and 3D transoesophageal echocardiography guidance. At the 30-day follow-up, echocardiography revealed a stable position of the MitraClip device with no MR.4 Yap et al. used transthoracic and intracardiac echocardiography to guide their MitraClip procedure. Severe MR was subsequently reduced to ≤2+ postoperatively.19 Improvement in heart failure symptoms was reported at a 30-day follow-up.19 Here, we report the third case of MTEER with an uneventful postprocedural course in a young OI patient with a favourable clinical course. In the above-mentioned three MTEER cases, no complications were reported.
Conclusion
MTEER could potentially serve as a suitable alternative to conventional surgery in OI patients with severe MR. Further studies are warranted to investigate the durability and feasibility of transcatheter valve interventions in this complex patient population.