The concept of myocardial salvage has been described since the 1970s. Acute MI is survivable but its impact is time dependent because the ‘wavefront’ of tissue necrosis begins to spread from a small area of infarct after 40 minutes of coronary occlusion, plateauing at around 96 hours.1 Dr O’Neill commented on the difficulty researchers faced at the time to accurately measure infarct size in human patients to prove that a therapy could potentially reduce infarct, and recognised that a method to directly or indirectly measure infarct size was needed. In a 1981 study that used systolic time intervals to estimate left ventricular (LV) viability, it was found that patients who had preserved LV systolic function following MI had superior 5-year survival.2 These findings supported the notion that patients who survived acute MI with a large infarct scar had poor long-term prognosis and led to a scientific pursuit of therapies to decrease infarct size.
Dr O’Neill shared his experience in his first randomised trial for streptokinase, conducted in 1983, that compared the intracoronary administration of streptokinase versus dextrose placebo within 6 hours from the onset of symptoms of acute MI in 40 patients.3 Although streptokinase achieved re-establishment of flow in 60% of patients, compared with 10% of patients in the control group, there was no statistically significant improvement in LV function measured by LV ejection fraction (EF).3 Following this, a study conducted in 2005 examined advanced imaging techniques as a means to determine the size of infarction. That study demonstrated the time dependency of salvage in patients with anterior infarction.4 For patients who presented within 2 hours of symptom onset, infarct size remained relatively small and rapid reopening of the artery could effectively decrease infarct size. However, this window of opportunity to salvage the myocardium rapidly diminished after 3 hours, after which there was limited scope for improvement in infarct size.4 In the US, the median time from symptom onset to presentation is 4.0 (IQR 1.6–16.0) hours.5 With the recommended door-to-balloon (DTB) time of 90 minutes, the total time from onset to reperfusion can be between 3.0 and 17.5 hours from symptom onset.6 This may be one of the reasons why, even though DTB time has improved markedly in the US over the past 20 years, it has had minimum impact on long-term survival. Therefore, in Dr O’Neill’s opinion, the biggest challenge is to treat patients within the time frame in which reperfusion can make a difference.
Given the practical difficulties in achieving this, an alternative strategy is to devise time-independent methods to decrease infarct size and improve myocardial function and salvage. In hearts with small infarcts, the apex may remain hypokinetic but the rest of the myocardium has the potential to positively remodel and recover. However, in hearts with large infarcts, both the apex and anterior wall become akinetic, with sequelae of adverse remodelling and ventricular dilation, leaving only a small potential for myocardial recovery.7 Therefore, the goal should be to decrease the infarct size enough so that the ventricle can positively remodel following the insult.
Dr O’Neill discussed data from the CRISP-AMI randomised trial that showed that among patients with acute anterior ST-elevation MI (STEMI) without shock, intra-aortic balloon counter-pulsation plus primary percutaneous coronary intervention (PCI) compared with PCI alone did not result in reduced infarct size.8 In contrast, the AMIHOT I + II trials showed that among patients with anterior STEMI undergoing PCI within 6 hours of symptom onset, the infusion of supersaturated oxygen into the left anterior descending artery infarct territory resulted in a significant reduction in infarct size.9,10
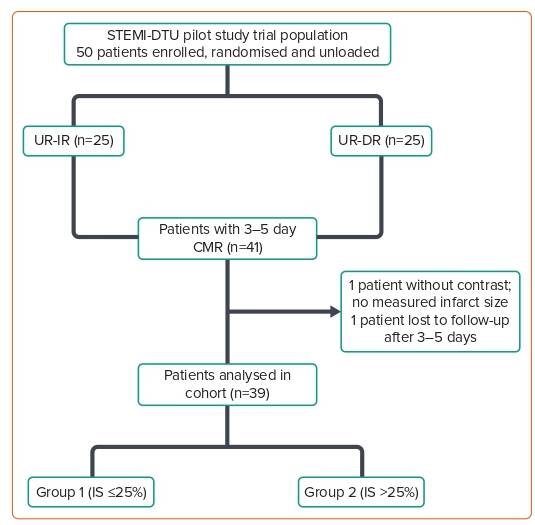
Dr O’Neill presented the STEMI-DTU pilot study, a multicentre prospective randomised safety and feasibility trial.9 In all, 50 patients were enrolled and randomised 1 : 1 to LV unloading with the Impella CP followed by immediate reperfusion (UR-IR arm) versus delayed reperfusion after 30 minutes of unloading (UR-DR arm). Forty-one patients were assessed by cardiac MRI (CMR) at 3–5 days and 30 days after PCI; 39 were analysed for the final analysis (Figure 1).
In order to assess the impact of the initial infarct size on heart recovery, the pilot study subjects were divided according to their infarct size measured by CMR 3–5 days after PCI into two groups: those with an infarct size measuring ≤25% LV mass and those with infarct size >25% LV mass. Results from the 30-day CMR and 90-day echocardiogram showed that the group with smaller initial infarct size experienced a greater increase in LVEF. For those with an initial infarct size >25% LV mass, LVEF remained flat at 30 and 90 days. These individuals also exhibited a significant increase in LV end-systolic and end-systolic volumes, indicating that the ventricle began to adversely remodel and dilate.11
Dr O’Neill also shared the echocardiogram-based wall motion analysis of the STEMI-DTU pilot cohort. The wall motion analysis showed that in patients with a larger infarct size (>25% LV mass), all three sections of the myocardium (basal, mid-cavity and apical) had significant proportions of hypokinesis and akinesis at 3–5 days. In the group with smaller (≤25% LV mass) infarct size, all three sections showed a significant proportion of hypokinesis, but a smaller proportion of akinesis and a larger proportion of normal wall motion compared with the group with larger infarct size. At 90 days, the group with smaller infarct size showed recovery to fully normal basal and nearly normal mid-cavity, with approximately 25% of patients with a hypokinetic or akinetic apex. In the group with large infarct size, the wall motion in the basal and mid-cavity at 90 days was largely hypokinetic, and the wall motion of the apex did not improve; 80% remained akinetic. These data show that if the anterior wall was akinetic in the period 3–5 days after injury, it was unlikely to be recoverable.
The aim is that patients are discharged from hospital with infarct sizes ≤25% of their LV mass. Current STEMI-DTU roll-in experience shows that two-thirds of patients enrolled are achieving infarct size ≤25%. Although not part of the original assessment, the study team will continue to monitor this.
Dr O’Neill summarised his presentation by reiterating that early revascularisation is the most potent intervention possible for improvement in survival outcomes, but unfortunately most patients do not present quickly enough to benefit from revascularisation. Multiple strategies have failed to limit infarct size, although intracoronary adenosine and supersaturated oxygen are potential therapeutic treatments. Dr O’Neill believes that unloading in the setting of STEMI offers enormous promise and feels optimistic about the findings that will come from the STEMI-DTU pivotal study.